Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 3 - May / June of 2007
Vol. 40 nº 3 - May / June of 2007
|
ORIGINAL ARTICLE
|
|
Radiological and epidemiological aspects of central giant cell granuloma |
|
|
Autho(rs): José Wilson Noleto, Edson Marchiori, Renato Kobler Sampaio, Klaus L. Irion, Felipe Birchal Collares |
|
|
Keywords: Central giant cell granuloma, Radiological aspects, Brown tumor, Hyperparathyroidism |
|
|
Abstract:
IFellow Master degree in Radiology, Universidade Federal do Rio de Janeiro (UFRJ), Oral and Maxillofacial Surgery Specialist by Universidade do Estado do Rio de Janeiro (UERJ), Rio de Janeiro, RJ, Brazil
INTRODUCTION Many maxillary lesions present similar histological patterns, especially in the presence of giant cells. This group of lesions includes central giant cell granuloma (CGCG), giant cell tumor of long bones, aneurysmatic bone cyst, brown tumor of hyperparathyroidism and the early stages of cherubism. Most of these diseases can be differentiated by the combination of clinical and radiological findings, but differentiation between CGCG and brown tumors of hyperparathyroidism only can be made by means of laboratory tests(1–3). CGCG is a non-neoplastic lesion of the jaws(4) that can present different radiological features, from small, unilocular radiolucent lesions to extensive multilocular radiolucent areas. Generally, the lesions are well circumscribed, many times presenting with festooned borders. They may present a cortical radiopaque halo and cause dental displacement or resorption. Such features are non-specific for confirming the diagnosis, and may be confused with other pathological lesions whose treatment is different(5–9). The present study was aimed at evaluating epidemiological and radiological characteristics of 26 giant cell lesions, including CGCG and brown tumors of hyperparathyroidism.
MATERIALS AND METHODS Epidemiological and radiological aspects of 26 cases of giant cell lesions in 22 patients of the Service of Oral and Maxillofacial Surgery at Hospital Universitário Pedro Ernesto – Universidade do Estado do Rio de Janeiro, were retrospectively evaluated. In the period between January/1990 and June/2004, 2,252 biopsies of maxillary or mandibular lesions were performed, 26 of them (1.1%) corresponding to giant cell lesions. All of the diagnoses were histopathologically confirmed. The patients were divided into two groups: group A, including patients with no evidence of hyperparathyroidism (n = 17), while group B included those with such a condition (n = 5). For differentiation between groups, the patients were submitted to evaluation of calcium, phosphorus, alkaline phosphatase and parathormone (PTH) serum levels. As regards epidemiological aspects, the prevalence according to patients´ age and gender, number of lesions, besides the presence of symptoms, was considered. Regarding radiological aspects, CT studies, extra-oral radiographs (panoramic, posteroanterior view, Water's view), and intra-oral radiographs (periapical and occlusal types). Radiographic images were classified according to the presence and number of loculations into unilocular radiolucent or multilocular radiolucent. Also, dental displacement, dental root resorption and cortical bone expansion were evaluated.
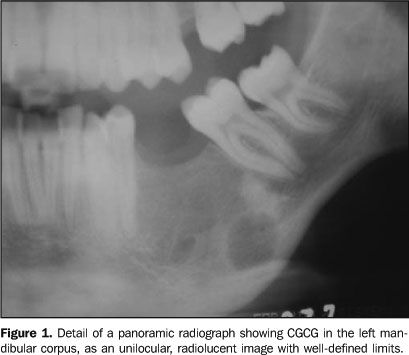
RESULTS Age, gender and symptoms Prevalence was higher in women (16 patients; 72.7%). In a comparison between groups, 12 patients of group A were women, and five were men. On the other hand, in group B, four patients were women, and one was men. The patients' ages ranged between five and 62 years, with higher incidence in the second decade of life. Mean age was 27 years. The age range of patients with hyperparathyroidism was 22–40 years (mean, 29.6 years). Only three patients (11.5%) presented with painful symptoms. Localization Of 26 diagnosed lesions, 16 (61.5%) affected the mandible, and 10 (38.5%) were associated with the maxilla. Of 16 giant cell lesions localized in the mandible, 12 (75%) were found in the mandibular corpus, three (18.7%) in the anterior region, and one (6.3%) in the mandibular ramus. In the maxilla, of 10 giant cell lesions, six (60%) were in the anterior region and four (40%) in the posterior region. Radiological features All of the 26 giant cell lesions evaluated in the present study showed up radiographically as a radiolucent image of well-delineated contour. Eleven lesions (42.3%) were unilocular (Figure 1), and 15 (57.7%), multilocular (Figure 2). The mandible presented nine (56.3%) multilocular lesions, and seven (43.7%) unilocular lesions. The maxilla presented six (60%) multilocular lesions, and four (40%) unilocular lesions) (Table 1).
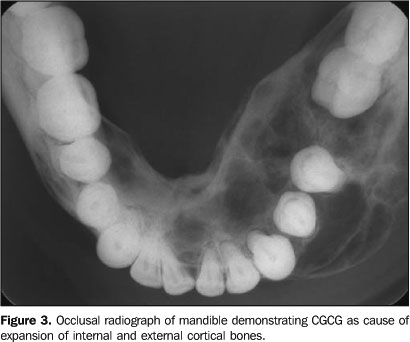
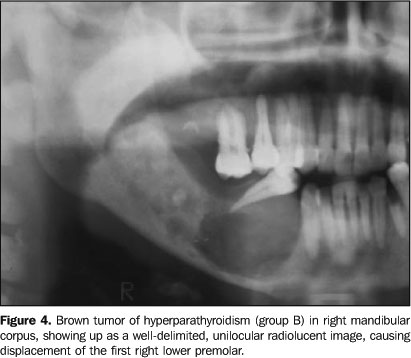
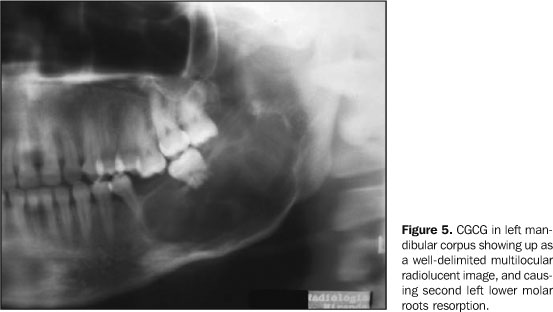
As regards the distribution of images among regions in the maxilla, three (50%) unilocular, and three (50%) multilocular lesions were found in the anterior region, and three (75%) multilocular lesions and only one (25%) unilocular, in the posterior region of the maxilla. The analysis of the radiographic images distribution between regions of the mandible showed seven (58.3%) multilocular, and five (41.7%) unilocular lesions in the mandibular corpus, and two (66.7%) multilocular lesions and one (33.3%) unilocular in the anterior region of the mandible. The only giant cell lesion in the mandibular ramus presented as a radiolucent multilocular image. At the level of the mandible, three (18.7%) of the 16 lesions crossed the midline. All of the lesions caused expansion of at least one cortical bone (Figure 3), 13 (50%) were associated with dental displacement (Figure 4), and four (15.4%) produced dental roots resorption (Figure 5). The evaluation of the involved cortical bone, 13 (50%) of the 26 giant cell lesions resulted in expansion of the internal cortical bone, and 24 (92.3%) in expansion of the external cortical bone.
DISCUSSION The mandible and the maxilla may be affected by non-neoplastic processes and bone tumors of several lineages(10–14). Very few bone lesions have caused more controversy than the CGCG, the giant cell bone tumor of long bone and the relationship between them. Before the fifties, the diagnosis of central giant cell tumor was usual for any bone lesion presenting giant cells(4,7,15,16). Presently, the majority of authors take the biological behavior and histological patterns into consideration in the differentiation between these lesions(1,4,15,17,18). Giant cell tumors of long bones present larger giant cells with more nuclei and more evenly distributed. Additionally, they present a high rate of recidivation after curettage, besides malignant alterations in about 10% of cases(7,15,17). The CGCG affects children and young adults, with more than 60% of cases occurring before 30 years of age(7,9). The majority of CGCGs is found in women(2,7,9). Our casuistic demonstrated prevalence in female patients in 72.7% of cases. Ages ranged between five and 62 years, with a higher incidence in the second decade of life, and mean age of 27 years, very similar to the literature(1,6,19–21). The CGCG is considered as an uncommon lesion of maxillas(7,22,23). Miniƒ & Staj…iƒ(19) have found 31 cases of CGCG (0.1%) in 29,134 biopsies performed in the period between 1970 and 1990. Waldron & Shafer(8) diagnosed 36 cases of CGCG (0.16%) in 22,000 specimens received by their laboratory. In the present study, 26 giant cell lesions (1.1%) were found in 2,252 biopsies performed in the period between Januray/1990 and June/2004. Eight (0.3%) of these 26 lesions were associated with patients affected by hyperparathyroidism (brown tumor) and 18 (0.8%), not. Mandible is more affected than maxilla, with the majority of lesions being found in the anterior region. The present study demonstrated that the mandible presented 61.5% of lesions diagnosed, and the maxilla, 38.5%, a result similar to the results presented in the literature(1,2,9,18–20,24). Bataineh et al.(20) reported that the molar/ramus (37%) is the most affected region, followed by the incisive/canine teeth region )28%), premolar/molar teeth region (22%), and premolar teeth region (11%). Cohen & Hertzanu(5) have reported the mandibular ramus (31%) as the most affected region, followed by the mandibular corpus (25%) and anterior (25%) regions. Our study demonstrated that of 16 mandibular lesions, 12 (74%) were in the region of the corpus, three (18.7%) were in the region of the symphysis, and one in the mandibular ramus (6.3%). Considering the corpus and ramus regions described as posterior in our sample, our results are similar to those reported in the literature(6,21,24,25). Cohen & Hertzanu(5), , in a sample of 16 cases of CGCG, reported three (18.7%) lesions in the maxilla, with two of them (66.4%) in the posterior region, and one (33.3%) in the anterior region, a result similar to the one reported by Sidhu et al.(25). On the other hand, in our study, of the 10 maxillary lesions (38.5%), six (60%) were in the anterior region, and four (40%), in the posterior region, a prevalence similar to the ones reported by other authors(24,26). Horner(24), Bodner & Bar-Ziv(22), and Cohen & Hertzanu(5) have reported that all of the lesions evaluated were radiolucent, with respectively 77%, 60% and 56,2% presenting well-defined limits. On the other hand, Stavropoulos & Katz(26) have studied 20 cases and observed that 55% of the lesions were radiolucent, 45% presented a mixed aspect, and 65% presented well-defined limits. Kaffe et al.(6) have observed 87.5% of studied CGCG as radiolucent images, 10% with mixed aspect, and 2.5% radiopaque. Although the literature demonstrates varied results, the present study demonstrated that the lesions presented radiographically as radiolucent images and with well-defined limits. Horner(24) and Austin et al.(1) have found, respectively, 85% and 97.1% of unilocular lesions. We observed that 15 (57.7%) of the 26 giant cell lesions of our sample produced multilocular images, and 11 (42.3%), unilocular images, a result similar to those of some authors(6,19,21). In the present study, nine (56.3%) of the 16 giant cell lesions in the mandible presented a multilocular image, and seven (43.7%), unilocular. In the maxilla, six lesions (60%) were multilocular, and four (40%), unilocular. In the case of unilocular lesions, they may look like periapical lesions, such as periapical cysts and granulomas(7,27). The literature highlights the possibility of radicular resorption as a result of CGCG(1,7,9,24). Horner(24), Kaffe et al.(6) and Stavropoulos & Katz(26) have found, respectively, 7.7%, 12% and 37% of radicular resorption. Our sample showed dental roots resorption in 15.4% of cases. The majority of CGCGs are asymptomatic, and usually are discovered during routine radiological examinations or because of the asymmetry caused by cortical bone expansion(2,7,9,24,25). In our sample, all of the 26 lesions caused expansion of at least one cortical bone, a result similar to the results presented in the literature 5,6,19,24,25). CGCGs present a tendency to cross the midline, principally when the lesion is in the mandible(7,9,21,28). In the present study, we observed that 18.7% of lesions crossed the midline, a result similar to those reported by some authors(5,20,25). Goaz & White(9) have pointed out that CGCG affecting the maxillary sinus may expand or erode bone walls, and are confused with tumors or mucoceles. The literature5,9,22) advises the utilization of computed tomography in these cases, aiming at evaluate more accurately the limits and the extension of the lesion through adjacent tissues. Painful symptoms are usual in cases de CGCG(6,9,21,24). Austin et al.(1) and Bodner & Bar-Ziv(22) have observed that, respectively 25% and 30% of their cases presented pain. In our study, we observed that 11.5% of cases presented painful symptoms. Dental displacement is a sign frequently associated with CGCG(2,5,21,22,25). Our sample demonstrated that 50% of cases produced adjacent teeth displacement, a result similar to those reported by some authors(6,24,26). Clinical, radiological and histological features of CGCG are identical to those found in brown tumors associated with hyperparathyroidism. These later may generate uni- or multilocular radiolucent images, showing up in approximately 10% of patients with hyperparathyroidism. The differentiation between these lesions depends on laboratory tests for investigating serum levels of calcium, phosphorus and alkaline phosphatase which, in cases of hyperparathyroidism, present alterations(3,9). Mandible and/or maxilla are sites where giant cell lesions develop in cases of hyperparathyroidism, many times as the first clinical manifestation of this disorder(28,29). Our sample demonstrated that 80% of patients with hyperparathyroidism were asymptomatic. Regezi(2) reports that hyperparathyroidism should be considered whenever facial bones are involved, in cases of recurrence, and in cases of multiple lesions. In the five patients affected by hyperparathyroidism, eight lesions were diagnosed. Three patients presented only one lesion. This demonstrates that not always will the patient with hyperparathyroidism present multiple lesions, and a patient may rarely present more than one lesion without hyperparathyroidism(28,29). Neville et al.(7) have reported that hyperparathyroidism affects women about two to four times more than men. Our sample demonstrated that four of five patients with hyperparathyroidism were women. The ages of patients with hyperparathyroidism ranged between 22 and 40 years (mean, 29.6 years). Evaluating the most affected maxilla in each group, we have found that 66.7% of lesions in group A were in the mandible. On the other hand, in group B, we have observed an even distribution — 50% for each arch. Based on the present data, we conclude that the knowledge about the variation of radiological images of CGCGs and brown tumors associated with hyperparathyroidism is extremely important. In case of patients with diagnosis of CGCG, the possible presence of parathyroid disorders should not be disregarded.
REFERENCES 1. Austin LT Jr, Dahlin DC, Royer RQ. Giant-cell reparative granuloma and related conditions affecting the jawbones. Oral Surg Oral Med Oral Pathol 1959;12:1285–1295. [ ] 2. Regezi JA. Odontogenic cysts, odontogenic tumors, fibroosseous, and giant cell lesions of the jaws. Mod Pathol 2002;15:331–341. [ ] 3. Som PM, Lawson W, Cohen BA. Giant-cell lesions of the facial bones. Radiology 1983;147: 129–134. [ ] 4. Jaffe HL. Giant-cell reparative granuloma, traumatic bone cyst, and fibrous (fibro-osseous) dysplasia of the jawbones. Oral Surg Oral Med Oral Pathol 1953;6:159–175. [ ] 5. Cohen MA, Hertzanu Y. Radiologic features, including those seen with computed tomography, of central giant cell granuloma of the jaws. Oral Surg Oral Med Oral Pathol 1988;65:255–261. [ ] 6. Kaffe I, Ardekian L, Taicher S, Littner MM, Buchner A. Radiologic features of central giant cell granuloma of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;81:720–726. [ ] 7. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 2nd ed. Philadelphia, PA: WB Saunders, 2002;522–525,695–697. [ ] 8. Waldron CA, Shafer WG. The central giant cell reparative granuloma of the jaws. An analysis of 38 cases. Am J Clin Pathol 1966;45:437–447. [ ] 9. Goaz PW, White SC. Oral radiology: principles and interpretation. 3rd ed. St. Louis, MO: CV Mosby, 1994;514–518,536–537. [ ] 10. Sá ACD, Zardo M, Paes Junior AJO, et al. Ameloblastoma da mandíbula: relato de dois casos. Radiol Bras 2004;37:465–468. [ ] 11. Botelho RA, Tornin OS, Yamashiro I, et al. Características tomográficas da displasia fibrosa craniofacial: estudo retrospectivo de 14 casos. Radiol Bras 2006;39:269–272. [ ] 12. Carvalho TN, Araújo Júnior CR, Costa MAB, et al. Querubismo: relato de caso e revisão da literatura com aspectos imaginológicos. Radiol Bras 2004;37:215–217. [ ] 13. Araújo Júnior CR, Carvalho TN, Fraguas Filho SR, et al. Tumor neuroectodérmico melanocítico da infância (progonoma): relato de caso enfatizando os aspectos tomográficos e revisão da literatura. Radiol Bras 2004;37:457–460. [ ] 14. Catalan J, Fonte AC, Lusa JRB, et al. Tumor de células gigantes ósseo: aspectos clínicos e radiográficos de 115 casos. Radiol Bras 2006;39:119–122. [ ] 15. Franklin CD, Craig GT, Smith CJ. Quantitative analysis of histological parameters in giant cell lesions of the jaws and long bones. Histopathology 1979;3:511–522. [ ] 16. Kaban LB, Troulis MJ, Ebb D, August M, Hornicek FJ, Dodson TB. Antiangiogenic therapy with interferon alpha for giant cell lesions of the jaws. J Oral Maxillofac Surg 2002;60:1103–1113. [ ] 17. Abrams B, Shear M. A histological comparison of the giant cells in the central giant cell granuloma of the jaws and the giant cell tumor of long bone. J Oral Pathol 1974;3:217–223. [ ] 18. Auclair PL, Cuenin P, Kratochvil FJ, Slater LJ, Ellis GL. A clinical and histomorphologic comparison of the central giant cell granuloma and the giant cell tumor. Oral Surg Oral Med Oral Pathol 1988;66:197–208. [ ] 19. Minic A, Stajcic Z. Prognostic significance of cortical perforation in the recurrence of central giant cell granulomas of the jaws. J Craniomaxillofac Surg 1996;24:104–108. [ ] 20. Bataineh AB, Al-Khateeb T, Rawashdeh MA. The surgical treatment of central giant cell granuloma of the mandible. J Oral Maxillofac Surg 2002;60: 756–761. [ ] 21. Whitaker SB, Waldron CA. Central giant cell lesions of the jaws. A clinical, radiologic, and histopathologic study. Oral Surg Oral Med Oral Pathol 1993;75:199–208. [ ] 22. Bodner L, Bar-Ziv J. Radiographic features of central giant cell granuloma of the jaws in children. Pediatr Radiol 1996;26:148–151. [ ] 23. Chuong R, Kaban LB, Kozakewich H, Perez-Atayde A. Central giant cell lesions of the jaws: a clinicopathologic study. J Oral Maxillofac Surg 1986;44:708–713. [ ] 24. Horner K. Central giant cell granuloma of the jaws: a clinico-radiological study. Clin Radiol 1989;40:622–626. [ ] 25. Sidhu MS, Parkash H, Sidhu SS. Central giant cell granuloma of jaws: review of 19 cases. Br J Oral Maxillofac Surg 1995;33:43–46. [ ] 26. Stavropoulos F, Katz J. Central giant cell granulomas: a systematic review of the radiographic characteristics with the addition of 20 new cases. Dentomaxillofac Radiol 2002;31:213–217. [ ] 27. Dahlkemper P, Wolcott JF, Pringle GA, Hicks ML. Periapical central giant cell granuloma: a potential endodontic misdiagnosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:739–745. [ ] 28. Goshen O, Aviel-Ronen S, Dori S, Talmi YP. Brown tumour of hyperparathyroidism in the mandible associated with atypical parathyroid adenoma. J Laryngol Otol 2000;114:302–304. [ ] 29. Smith PG, Marrogi AJ, Delfino JJ. Multifocal central giant cell lesions of the maxillofacial skeleton: a case report. J Oral Maxillofac Surg 1990;48: 300–305. [ ]
Received July 26, 2006.
* Study developed at Department of Radiology of Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554