Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 1 - Jan. /Feb. of 2007
Vol. 40 nº 1 - Jan. /Feb. of 2007
|
REVIEW ARTICLE
|
|
Sacroiliitis: imaging evaluation |
|
|
Autho(rs): Cristiano Montandon, Marlos Augusto Bitencourt Costa, Tarcísio Nunes Carvalho, Marcelo Eustáquio Montandon Júnior, Kim-Ir-Sen Santos Teixeira |
|
|
Keywords: Sacroiliitis, Spondyloarthropathy, X-ray, Computed tomography, Magnetic resonance imaging |
|
|
Abstract:
IMDs, Radiologists at Clínicas da Imagem e Multimagem, Titular Members of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
INTRODUCTION The sacroiliac joints are frequent sites of lumbar pain orlumbosciatalgia commonly seen in the clinical daily practice, anon-infectious inflammatory process — sacroiliitis —being the most frequent cause of disease in thistopography(1). Seronegative spondyloarthropathies are basically subdividedand differentiated by their clinical features, and are classifiedinto five different entities: ankylosing spondylitis, reactivearthritis, psoriatic arthritis, arthritis related with chronicinflammatory disease and undifferentiated spondyloarthropathy.The inflammatory involvement of sacroiliac joints is a criterionfor diagnosis of these diseases(1–3). Most frequently, spondyloarthropathies occur in youngpatients, the early diagnosis being critical for establishment ofan appropriate therapy aiming at improving prognosis and workingcapacity of the patients(3). Most of times, the clinical diagnosis of sacroiliitis isdifficult, depending substantially on the confirmation ofradiological findings, where conventional x-ray, and currently,computerized tomography (CT) and magnetic resonance imaging (MRI)assume na essential role(4–6). The objective of the present study was to review anddemonstrate the main aspects in sacroiliac joints imagingevaluation, especially on CT and MRI.
MATERIALS AND METHODS Twenty-five cases with different imaging studies forsacroiliac joints evaluation have been retrospectively selectedfrom the files of Clínicas da Imagem e Multimagem,Goiânia, GO, Brazil, aiming at didactically illustratingthe anatomy, technique and findings of the main conditionsaffecting these joints. The studies were performed in equipmentof different brands. X-rays images were obtained in anteroposterior views with caudal and oblique inclinations. The current protocol for CT studies consists of axial and coronal oblique images acquisition in 3.0 mm-thick slices, guided by digital radiography, without contrast agent injection (Figure 1).
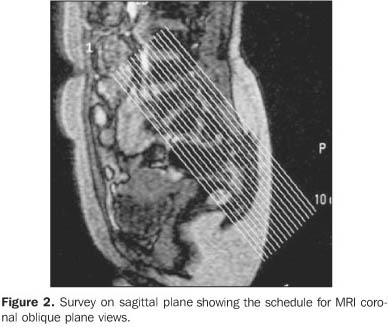
The protocol for MRI also consists of axial and coronal oblique views in 4.0 mm-thick slices, with narrow view field (20–24 cm) and 256 × 512 matrix, in T1, T2-weighted and STIR sequences. Later, T1-weighted sequences with fat saturation are performed, before and after gadolinium injection (Figure 2).
It was not a purpose of this study a systematic analysis ofeach case separately.
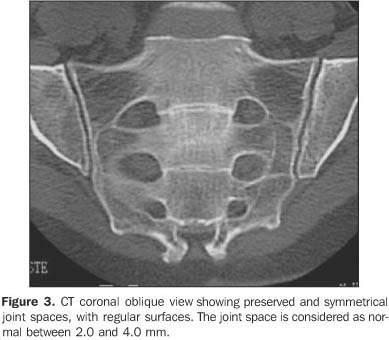
DISCUSSION The sacroiliac joint presents a complex two-compartmentanatomy. The synovial portion of the sacroiliac joint isvertically oriented, while the ligamentous portion presentshorizontal-oblique orientation(4,5). Puhakka etal. have demonstrated that, histologically, the synovial portionis a symphysis with some characteristics of a synovial jointbeing confined to the distal cartilaginous portion at the iliacside(7). Several studies indicate that the vertical synovial tissue isbetter demonstrated by coronal, obliqueviews(1,4–6). Puhakka et al. have demonstratedthat axial, oblique views provide a better visualization of thetwo-compartment anatomy of this joint, as well as of someanatomic variations, facilitating the interpretation of imagingfindings(7). The normal joint space of the sacroiliac joint measures 2.5–4.0 mm (mean = 3.0 mm)(4,5) (Figure 3).
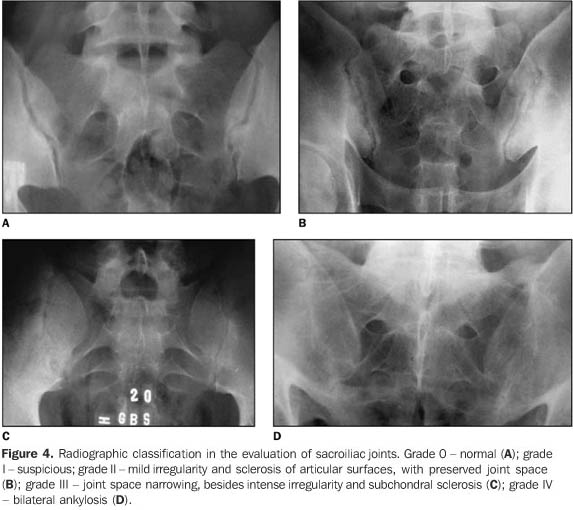
Conventional x-ray still remains as the imaging method mostutilized in the clinical practice. An international consensusstill remains to be reached regarding the best technique and viewfor radiographic evaluation of the sacroiliac joint.Anteroposterior views with 25–30º caudal angulation of thex-ray tube, and oblique views are the most utilized in ourpractice, in an attempt to minimize structures overlapping, sofacilitating the study interpretation(1,6). The main limitation of the x-ray film is the low sensitivityfor detecting abnormalities in the early stages of the disease.Radiographic signs in sacroiliitis appear only three to sevenyears after the initial symptoms onset, presenting withalterations only in the chronic phase of thedisease(1,2,8). The main radiographic signs are: bone erosions, joint spacealterations, subchondral sclerosis andankylosis(6,8–11). Assessing a patient with suspected sacroiliitis, we may classify the sacroiliac joint into five radiographic grades (modified New York criterion): 0 – normal; 1 – suspect, although unclear alterations; 2 – minimal erosions and sclerosis, but without joint space alteration; 3 – erosions and sclerosis, with widening or narrowing of the joint space; 4 – ankylosis(1,6,9,10) (Figure 4).
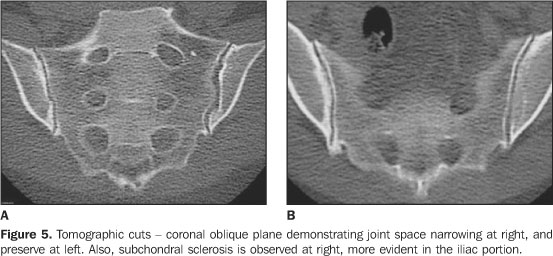
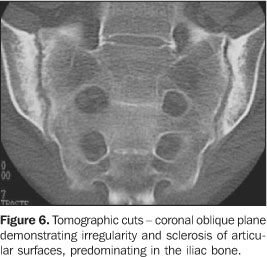
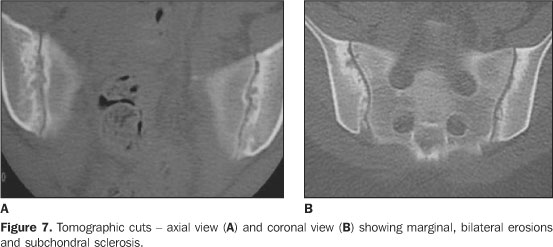
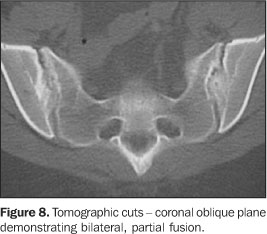
Scintigraphy presents high sensitivity for sacroiliitis, butspecificity is low. This study must be interpreted in combinationwith other radiological study, and is of higher value in cases ofunilateral alterations. The most significant indication would befor localizing another disease as a cause of lumbarpain(1,6,8). Imaging methods like CT and MRI are extremely useful,especially in the absence of alterations, or when they areminimal on plain x-ray (grades 0 to 2)(1). The evaluation of sacroiliitis by CT, in comparison with theconventional x-ray, has shown to be more sensitive, with a betterand earlier detection of bone alterations, principally because ofits capability to perform sequential slices, so avoidingstructures overlapping(6,7,9,10,12). The CT shows higher sensitivity for detecting minimal boneerosions and joint space narrowing, however presents the samediagnostic capacity of plain x-rays in cases ofankylosis(2). Lawson et al. have not found anyabnormality on x-ray films that were not defined byCT(5). The most frequent findings of sacroiliitis on CT are: joint space narrowing, subchondral sclerosis, bone erosions and ankylosis. Joint space narrowing is characterized by a thickness of less than 2.0 mm in synovial tissues (Figure 5). Subchondral sclerosis is found in the presence of an asymmetrical or focal area with increased density (> 5.0 mm on the iliac side, and > 3.0 mm on the sacral side) (Figure 6). Bone erosions are small cortical defects on the synovial portion of the joint (Figure 7). These two latter findings can be seen in both sides of the joint, however, they are frequently seen at the iliac side because this side presents lower thickness and some cartilaginous clefts. The focal or complete fusion of the joint characterizes ankylosis observed in more advanced stages of the disease(4,5) (Figure 8).
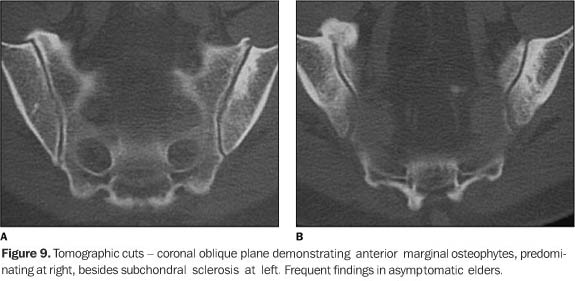
Alterations in the ligamentous portion are rare, when comparedwith the synovial portions. CT is better than MRI for detectingbone formation in the enthesis of thistopography(3). CT is comparable to MRI for detecting bone erosion, but issuperior for evaluating bone sclerosis and ankylosis, and isindicated especially for detecting chronicalterations(1). CT is a method of excellence in demonstrating bone details,besides serving as a guidance tool in percutaneous biopsies,arthrocentesis, and for intra-articular injection ofsteroids(6,11,12). On the other hand, sacroiliac evaluations by CT presents someinconveniences like radiation exposure, and incapacity to showalterations in the acute phase, identifying especially theinflammation consequences rather than the inflammatory processactivity(2,6,8–10). Elgafy et al. have demonstrated lower sensitivity and specificity of CT in the evaluation of patients with suspected pain in the sacroiliac joint, since asymptomatic patients, especially the oldest ones, present some findings similar to those of sacroiliitis, like marginal osteophytes and subchondral sclerosis(4) (Figure 9).
MRI has been suggested as a method of choice in the evaluationof sacroiliitis, because of the higher quality of the images,absence of ionizing radiation, and mainly the capacity ofdetecting and differentiating acute and chronicalterations(2,6,8–11). Structures comprising the sacroiliac joint are better demonstrated by MRI, and are seen as follows: 1) cartilage – a thin zone of intermediary signal on T1- and low signal on T2-wieghted sequences, with high signal on T1-weighted, fat-saturated sequences; 2) subchondral cortex – linear zone with signal void on T1- and T2-weighted sequences, is better seen on T1-weighted, fat saturated sequences; 3) subchondral medullary – homogeneous, intermediary signal on T1- and T2-weighted, and low signal on fat-saturated and STIR sequences; 4) absence of bone marrow uptake after intravenous contrast injection (gadolinium)(2,4,7) (Figure 10).
Main alterations seen on MRI of patients with sacroiliitis are(2,6,8–11) (Table 1):
a) Interarticular fluid collection – is better seen on T2, mainly on T2-weighted, fat-saturated and STIR sequences (Figure 11);
b) replacement of articular cartilage by pannus (synovial proliferation), resulting in heterogeneous signal, with areas of focal thickening with hypersignal on T2-weighted sequences and contrast uptake (Figure 12); c) cortical bone erosions represented by foci with highintensity or intermediary signal on T1- and T2-weighted sequencesin sacral or iliac cortical bones, with marginal irregularity anddeeper defects, also affecting the adjacent bone marrow. Theseerosions are better demonstrated on T1-weighted fat-saturatedsequences; d) subchondral sclerosis characterized by zones withlow-intensity signal on T1- and T2-weighted images; e) subchondral bone marrow edema characterized by low-intensity signal on T1- and high-intensity signal on T2-, especially the T2-weighted fat-saturated and STIR sequences. On T1-weighted fat-saturated sequences, after intravenous gadolinium injection, a significant enhancement of sacroiliac joint and surrounding bone marrow can be observed, and this finding is highly suggestive of an active disease (Figure 12); f) signs of focal or diffuse, periarticular in chronic phases, bone marrow reconversion (fat collection) (Figure 13);
g) bone ankylosis represented by low-intensity signal throughthe sacroiliac joint, permeated by areas of intermediary signrepresenting bone marrow. In 1990, Ahlström et al.(13) describedtwo types of lesions identified by MRI. Type I lesions werecharacterized by low-intensity on T1-weighted, and high-intensitysignals on T2-weighted sequences and on images acquired aftergadolinium injection. Type II lesions were characterized bylow-intensity signal in all of the sequences. This observationhas suggested that MRI is able to differentiate lesions with highhydric contents (inflammatory edema) from those with fibroustissue or sclerosis, i.e., differentiating acute from chronicalterations. Type II lesions are associated with fatcollections(13). The study developed by Hanly et al.(9) hasproposed that subchondral bone marrow edema is the earliestmanifestation of the acute sacroiliitis, since 57% of theirpatients with subchondral bone edema did not present any sign ofarticular cartilaginous alteration. This theory ishistopathologically corroborated by another study, by means ofopen biopsy in patients with initial stage of disease, where theearliest finding was subchondral inflammation. The sequence withhighest sensitivity and specificity in detecting periarticularbone marrow edema is the STIR sequence, since, differently fromthe conventional T2-weighted spin-echo sequence, it saturates defat, differentiating it from fluid(6,8,12). The limitation of this finding — subchondral bone marrowedema — is that it also occurs in early phases of thedegenerative process resulting from vascularization of fibroustissue. For differentiating them, it is important to observe thesite of the edema, i.e., hypersignal on the synovial portion ofthe sacroiliac joint indicates inflammatory disease, and, on theligamentous portion, indicates degenerativedisease(8). The use of dynamic post-contrast sequence in the evaluation ofinflammatory processes has been reported in several studies, butthis has not been easily done in the dailypractice(3). Puhakka et al. have demonstrated some anatomical variations,like synovial recesses, bony and cartilage clefts, situated inthe transition between the two proximal one-thirds and the distalone-third of the dorsal aspect of the iliac side of the jointthat may mimic bone erosion, contrast-enhancement on theligamentous portions as a result of the intense vascularization,and fat infiltration of the sacral bone marrow withoutpathological significance(7). Oostveen et al. have demonstrated a 60% positive predictivevalue of MRI for sacroiliitis development after three years, with85% sensitivity and 47% specificity(14). On theother hand, Battafarano et al. have demonstrated high MRIsensitivity and specificity (100%) for type I alterations, and,respectively 69% and 46%, in the evaluation of type IIalterations. The main disadvantages of MRI are: high cost, lowavailability, and long duration of examination (30 minutes),although the latter is well tolerated by the majority ofpatients, in pediatric examinationsincluded(1,2,6,11).
DIFFERENTIAL DIAGNOSES The main differential radiographic diagnosis of sacroiliitis is condensing iliac osteitis, that usually presents bilaterally and symmetrically in female, asymptomatic patients, manifesting on images as sclerosis of the ventro-caudal portions of the sacroiliac joint(14) (Figure 14).
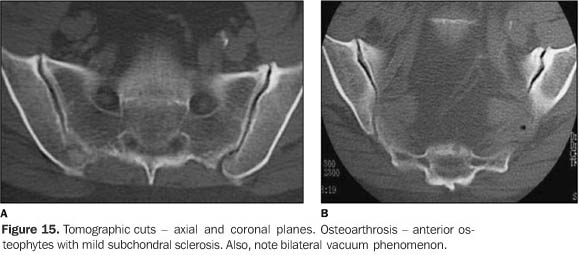
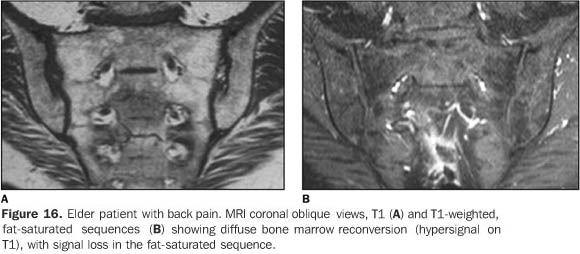
Other relevant differential radiographic diagnoses includemetabolic diseases like hyperparathyroidism and gout. Usually, incases of hyperparathyroidism the condition manifests bilaterallyand symmetrically, either in its primary form or in its secondaryforma (renal osteodystrophy), characterized by subchondral bonereabsorption with irregularity on the bone surface, sometimeswith adjacent sclerosis and widening of the joint space. In casesof chronic tophaceous gout, the condition may manifestsymmetrically or asymmetrically, sometimes unilateral,characterized by large, destructive erosion with a sclerotichalo, but with preserved join space(15). In the evaluation of the sacroiliac joint, the patient 's age should be taken into consideration, since osteoarthrosis is frequent in elder, asymptomatic patients. These alterations are characterized by marginal osteophytes, subchondral sclerosis, and eventually articular fusion(1,3) (Figure 15). Erosion, subchondral cysts and ankylosis are rarely seen in the degenerative process(4). Early in the initial phase of the process, periarticular subchondral bone marrow edema can be seen representing fibrous, vascularized tissue(8). Fat deposition also may be seen in normal elder individuals, and in patients with degenerative disease(16) (Figure 16).
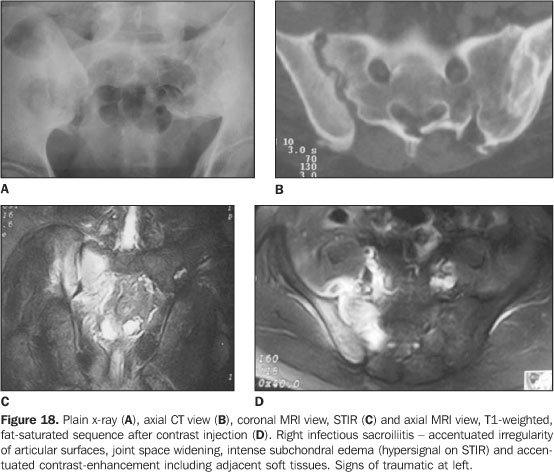
Other important differential diagnosis is infectioussacroiliitis, particularly the pyogenic type. Infectioussacroiliitis is quite rare, prevailing in injectable drugs usersand in individuals with skin, pulmonary and genitourinaryinfections, and have as its most frequent etiologic agent theStaphylococcus aureus. The diagnosis of infectioussacroiliitis is difficult, many times delayed because of itsinsidious clinical presentation with non-specific and poorlylocalized signs, frequently simulating abdominal syndromes,lumbar discopathies or lumbosciatalgia. CT and MRI allow anearlier diagnosis, but are not able to define the etiologicagent. Generally, radiographic alterations can be observed onlytwo or three weeks after the first symptoms onset, while oncontrast-enhanced MRI, alterations can be observed within up tothree days, showing MRI highersensitivity(2,6,15). CT findings in the infectious process are the same of those observed in the sacroiliitis of spondyloarthropathies, except for the juxtarticular bone demineralization, considered as the earliest finding, besides signs suggestive of soft tissues involvement and unilaterality of the process(12). MRI, besides determining alterations in the affected sacroiliac joint and in the contiguous bone, also clearly demonstrates the involvement of adjacent soft tissues or collections, frequently posteriorly to the iliopsoas muscle, these findings being highly suggestive of infectious involvement, and not seen in spondyloarthropathies(6,12,13,15,16) . The intravenous gadolinium injection can more accurately define these soft tissues involvement(12,13,16) (Figures 17 and 18).
CONCLUSION The conventional x-ray remains as the method of choice in theprimary evaluation and follow-up of patients with sacroiliitis.The MRI plays an essential role in better demonstrating earlyalterations and inflammatory activity of this process. On theother hand, CT is superior in quantifying chronicalterations.
REFERENCES 1.Braun J, van der Heijde D. Imaging and scoring in ankylosing spondylitis. Best Pract Res Clin Rheumatol 2002;16:573–604. [ ] 2.Oostveen JCM, van de Laar MAFJ. Magnetic resonance imaging in rheumatic disorders of the spine and sacroiliac joints. Semin Arthritis Rheum 2000;30:52–69. [ ] 3.Puhakka KB, Jurik AG, Egund N, et al. Imaging of sacroiliitis in early seronegative spondylarthropathy. Assessment of abnormalities by MR in comparison with radiography and CT. Acta Radiol 2003;44:218–229. [ ] 4.Elgafy H, Semaan HB, Ebraheim NA, Coombs RJ. Computed tomography findings in patients with sacroiliac pain. Clin Orthop Relat Res 2001; 382:112–118. [ ] 5.Lawson TL, Foley WD, Carrera GF, Berland LL. The sacroiliac joints: anatomic, plain roentgenographic, and computed tomographic analysis. J Comput Assist Tomogr 1982;6:307–314. [ ] 6.Braun J, Sieper J, Bollow M. Imaging of sacroiliitis. Clin Rheumatol 2000;19:51–57. [ ] 7.Puhakka KB, Melsen F, Jurik AG, Boel LW, Vesterby A, Egund N. MR imaging of the normal sacroiliac joint with correlation to histology. Skeletal Radiol 2004;33:15–28. [ ] 8.Battafarano DF, West SG, Rak KM, Fortenbery EJ, Chantelois AE. Comparison of bone scan, computed tomography, and magnetic resonance imaging in the diagnosis of active sacroiliitis. Semin Arthritis Rheum 1993;23:161–176. [ ] 9.Hanly JG, Mitchell MJ, Barnes DC, MacMillan L. Early recognition of sacroiliitis by magnetic resonance imaging and single photon emission computed tomography. J Rheumatol 1994;21: 2088–2095. [ ] 10.Blum U, Buitrago-Tellez C, Mundinger A, et al. Magnetic resonance imaging (MRI) for detection of active sacroiliitis: a prospective study comparing conventional radiography, scintigraphy, and contrast enhanced MRI. J Rheumatol 1996;23: 2107–2115. [ ] 11.Bollow M, Biedermann T, Kannenberg J, et al. Use of dynamic magnetic resonance imaging to detect sacroiliitis in HLA-B27 positive and negative children with juvenile arthritides. J Rheumatol 1998;25:556–564. [ ] 12.Bellussi A, Busi Rizzi E, Schininá V, De Santis A, Bibbolino C. STIR sequence in infectious sacroiliitis in three patients. Clin Imaging 2002; 26:212–215. [ ] 13.Ahlström H, Feltelius N, Nyman R, Hallgren R. Magnetic resonance imaging of sacroiliac joint inflammation. Arthritis Rheum 1990;33:1763–1769. [ ] 14.Oostveen J, Prevo R, den Boer J, van de Laar M. Early detection of sacroiliitis on magnetic resonance imaging and subsequent development of sacroiliitis on plain radiography. A prospective, longitudinal study. J Rheumatol 1999;26:1953–1958. [ ] 15.Resnick D. Bone and joint imaging. 2nd ed. Philadelphia: WB Saunders,1996. [ ] 16.Haliloglu M, Kleiman MB, Siddiqui AR, Cohen MD. Osteomyelitis and pyogenic infection of the sacroiliac joint. MRI findings and review. Pediatr Radiol 1994;24:333–335. [ ]
Received March 4, 2005.
* Study developed at Clínicas da Imagem e Multimagem, Goiânia, GO, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554