Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 6 - Nov. / Dec. of 2008
Vol. 41 nº 6 - Nov. / Dec. of 2008
|
ORIGINAL ARTICLE
|
|
Aid in the detection of myocardial perfusion abnormality utilizing SPECT atlas and images registration: preliminary results |
|
|
Autho(rs): Rodrigo Donizete Santana de Pádua, Lucas Ferrari de Oliveira, Paulo Mazzoncini de Azevedo Marques, Jean-Jacques Georges Soares de Groote, Adelson Antonio de Castro, Lauro Wichert Ana, Marcus Vinicius Simões |
|
|
Keywords: Scintigraphy, SPECT, Myocardium, Nuclear medicine, Computer-assisted image processing, Computer-assisted diagnosis |
|
|
Abstract:
IBachelor of Computational Science, Voluntary Researcher, Division of Cardiology and Unit of Nuclear Medicine at Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil
INTRODUCTION Digital medical imaging techniques associated with scientific and technological developments in the areas of images processing and graphic computation, have allowed the development of a range of computer-aided diagnosis – CAD systems. Besides improving the visualization and manipulation of medical images, such systems allow the quantification of the abnormalities detected(1,2). Among the nuclear medicine imaging techniques applied to cardiology, myocardial perfusion scintigraphy (MPS) with single photon emission computed tomography (SPECT) allows the acquisition of digital images demonstrating the relative radiopharmaceutical uptake in the left ventricular myocardium for noninvasive detection of ischemic or fibrotic areas resulting from ischemic cardiopathy. The study is performed with the patient under physical or pharmacological stress/rest conditions and the images acquisition is performed after a radiopharmaceutical injection into the patient's blood current. Most frequently, thallium-201 (201Tl) or technetium99m (99mTc)-sestamibi are utilized for this purpose. Then, the photons emitted by the radioactivity accumulated in the different segments of the target-organs are detected by the scintillation chamber crystals, quantified and processed for images generation(3,4). A technical issue inherent to the myocardial perfusion images acquisition by SPECT is the frequent presence of attenuation artifacts or false uptake defects resulting from the passage of photons through soft tissues. Dense breasts in women and subdiaphragmatic tissues in men are common causes for attenuation artifacts. The presence of these artifacts results in a significantly decreased diagnostic specificity of this imaging method(3). A technique called "transmission" utilizes an external radiation source for obtaining maps of correction and minimization of photon attenuation effects on the final image. However, the patients' exposure to the effects and risks of higher levels of ionizing radiation should be taken into consideration as a significant disadvantage of this technique(5). An alternative approach aimed at improving the diagnostic accuracy of the method is the utilization of computational algorithms for comparison of patients' images with normality standards based on images of a group of healthy individuals of the same genre, which allows a mathematical correction of attenuation artifacts. So, on the image of a determined patient, only those voxels with significantly lower uptake intensity as compared with the voxels on the template image (> two standard-deviations below the mean) strongly indicate the presence of regions with myocardial perfusion defects requiring further investigation. Classically, this quantitative analysis is performed by means of polar mapping. Although this approach has already been validated, differences between the visual representation of areas with perfusional defects by this technique and the traditional visualization of tomographic sections still represent a limitation to a more disseminated utilization of this method(6). Aiming at preserving the tomographic sections visualization in the quantitative analysis and visualization of perfusional defects, an alternative approach utilizing 3D image registration techniques is suggested for obtention of normal template images for comparison and later identification of perfusional defects on tomographic sections(7,8). Both the obtention of these template images and their comparison with patients' images require an intermediate processing phase corresponding to a spatial alignment between images that can be achieved with the utilization of medical images registration techniques(7). Basically, images registration is aimed at defining parameters for changing a "source" image in a way to achieve the best alignment possible with another image called "target image"(9–13). The present study describes the utilization of image registration and other techniques for digital images processing for the development of an atlas of myocardial perfusion scintigraphy, and evaluates the preliminary results of the utilization of such atlas as an aid in the detection of myocardial perfusion defects through the comparison between images. So, it is expected that the method applicability is evaluated for later development of a computer-aided design tool for cardiology as well as prospective studies involving a higher number of patients aiming at validating this method. Despite the commercial availability in the market of similar already validated applications, the local development of such tool can be useful for the author's institution in the reduction of costs with hardware and software licenses acquisition, as well as allowing a better integration with already implemented hospital and radiological information systems. Furthermore, the future implementation of refinements and customization of this tool is feasible, considering the possibility of reutilization of the source-code that will be already available, so encouraging a culture of research & development in information technology in the field of medical images.
MATERIALS AND METHODS Tomographic images acquisition and processing Aiming at obtaining the template images for the atlas, the authors selected stress/rest images of myocardial perfusion scintigraphy with 99mTc-sestamibi which were visually analyzed and considered as normal by two experienced observers based on the pattern of relative radiopharmaceutical accumulation in myocardial segments. The images were divided into categories according to the patients' genre and physiological condition as follows: male-rest, malestress, female-rest and female stress categories. In order to evaluate the feasibility and potential of this method as an aid in the detection of myocardial perfusion defects, rest/stress images of one adult man and one adult woman with reversible, moderate perfusional defects were selected for statistical comparison with the template images. Images acquisition for all the patients was performed with a DST-SMV dual-head digital gamma camera with a low-energy collimator and energy window with 20% centered on keV. Tomographic planes were acquired on a circular orbit covering 180º, with 32 projections (16/head) and 60 sec/projection. Projections were corrected according standards for field uniformity and rotational center. Then, a Butterworth filter (5th order, 0.25 cy/mm cutoff frequency) was utilized for construction of image sets. Subsequently, tomographic sections on classical orthogonal planes were automatically generated by a commercially available software. The images were converted into DICOM 3.0 format and transmitted to the workstation for processing. Images registration and obtention of template images for the atlas All the images were aligned in relation to a single coordinate space with the software pack VTK CISG Registration Toolkit (vtkCisg), developed by Hartkens et al.(14) and made freely available by the Computational Imaging Science Group of Kings College of London. The vtkCisg performs rigid and non-rigid images registration through voxels similarity, allowing the user the option for cross correlation – C), mutual information – MI, normalized mutual information – NMI measurements, among others. The rigid registration method was adopted to avoid anatomical deformation on the images, utilizing only scale, rotation and translation transformations, although there are other alternative non-rigid registration techniques(9,10,13). Figure 1 demonstrates the equation for measurement of voxels similarity by means of cross correlation utilized for images alignment.
In this equation, N corresponds to the number of voxels on each of the images, and A(i) and B(i) to the overlapping voxels intensity i respectively on the images A and B. It is important to note that, the higher the C value, the more an image overlaps the other, and two identical images should correspond to the value 1 (one). So, the image registration algorithm will generate parameters for spatial transformation of images performing several interactions until the C value achieves the nearest possible to 1(9). Once the images were spatially registered, the next step was the obtention of template images of the mean myocardial uptake rate for each gender/physiological condition. For this purpose, a software based on the Visualization Toolkit (VTK) library(15,16), called vtkImageAVG was developed. Through this software, n 3D medical images are entered and normalized according to a 100-level gray-scale, and a final image corresponding to a median image of all the normalized images is generated. The definition of the images normalization in a 100-level gray-scale is aimed at allowing a direct quantitative evaluation of the rate of myocardial perfusion defect based on the comparison of the patients' images with the respective values in the template images of the atlas. The gray-scale values indicate a maximum uptake at 100, with the normalization calculation corresponding to the division of the original image voxels value by the highest voxel, and subsequent multiplication of this result by 100. The statistical analysis of the myocardial perfusion cannot be performed only by comparison between the patient's image and the mean image of normal individuals. It is necessary to have template images reflecting the intensity variability found on images of normal individuals. A software called vtkImageSD was developed for this purpose. Based on n input images, this software generates template images reflecting the standard deviation of the individual's myocardial perfusion uptake rate. In the present study, four mean images and four standard deviation images were generated - one for each gender-physiological condition category. All of the images are normalized for 100 gray levels, so they can be compared with the patient's images normalized according to the same gray-scale. Algorithm for detection of perfusion defects The algorithm for statistical comparison between patients' images and appropriate genderphysiological condition template images consists of four elementary steps: 1) patient's image alignment with the corresponding template image with the mean myocardial perfusion uptake rate based on C; 2) patient's image normalization according to a 100-level gray-scale; 3) selection of patient's image voxels with myocardial uptake rates two standard deviations below the mean voxel value of the respective region; 4) construction of the myocardial perfusion defect image. Figure 2 illustrates the step in the algorithm where the selection of voxels on the perfusion defect images is performed. Note that P(i), AVG(i), SD(i) and DP(i) store respectively the overlapping voxels intensity on the patient's image, mean gender-physiological condition, standard-deviation for gender/physiological condition and perfusional defect images, with i ranging from 1 up to the total number of voxels N. If the P(i) value is different from de 0 (zero) and lower than the AVG(i) value less 2 x SD(i), then DP(i) corresponds to the perfusional defect rate; otherwise it corresponds to 0. Considering that the images are normalized according to a 100-level gray-scale, subtracting the P(i) value from 100 will be enough to have the perfusion defect rate.
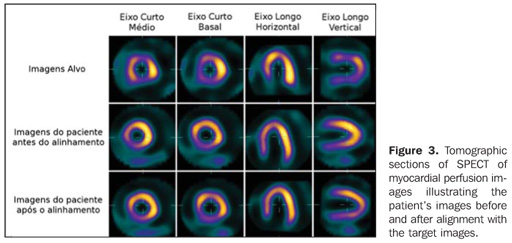
RESULTS Images registration Figure 3 illustrates the images alignment process adopted both for creating the atlas template images and for comparing the patients' images with the corresponding template images. One can observe tomographic sections of the three orthogonal axes (middle and basal short axis, vertical long axis and horizontal long axis): on the first range, views of the target-image; on the second, views of the patient's image before the alignment; and on the third range, views of the patient's image after alignment. By observing and comparing the landmarks at the center of each view, one can note that after the alignment, the patient's images are in the same coordinate space of the target image, differently from the images before the alignment.
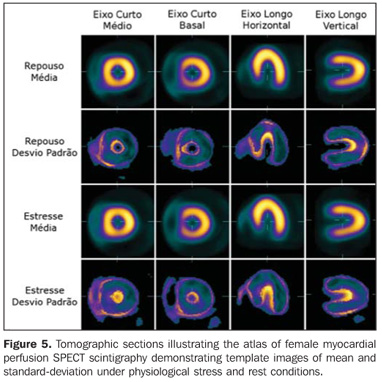
Construction of the normality atlas Through registration and addition of rest/stress images of ten female and ten male normal individuals, the authors obtained template images normalized according to a 100-level gray-scale representing the mean uptake and standard deviation for each voxel on the respective images. Figures 4 and 5 show SPECT images of the atlas of myocardial perfusion, with mean myocardial perfusion uptake rates and standard deviation. Images of mean uptake are similar to those of any male or female individual with low probability of myocardial ischemia. On the other hand, images of standard deviation present higher (clear) value on the borders where structural differences can be more clearly observed in the myocardium.
Perfusion defect detection Figures 6 and 7 illustrate the detection of myocardial perfusion defect for respectively male and female test-patients. The process for alignment of patients' images with the atlas template images, and generation of perfusion defect images for each genre-physiological condition took approximately 45-60 seconds in a standard PC (AMD Athlon XP-2000 processor, 1 Gb RAM, running operational system Ubuntu GNU/Linux version 8.04 LTS).
The first and third range of images on Figure 6 demonstrate three orthogonal axis of, respectively, rest/stress cardiac SPECT projections of the male patient already aligned with the template images of mean perfusion uptake for male individuals (Figure 4). The second range demonstrates the same projections overlapped by the perfusion defect image where arrows indicate the areas with myocardial perfusion abnormality. In the same way, the fourth range shows areas of perfusion abnormality with the patient under stress condition. Accordingly with the visual analysis performed by two experienced observers, the results indicate a reversible, extensive perfusional defect on the anterior, septal, apical and postero-lateral walls of the myocardium. Like Figure 6, Figure 7 demonstrates the female patient's images already aligned with the corresponding template images (Figure 5), besides presenting the areas with myocardial perfusion defect indicated by the arrows. Also, in complete agreement with the visual analysis results, the automatic detection technique indicates a reversible perfusional defect in the apical region and postero-lateral wall.
DISCUSSION Images registration has played an essential role in the development of the present study, both in the construction of template images and in their statistical comparison with patients' images. This process is necessary because of the tomographic images reconstruction where the human operator cannot accurately define the sections positioning in a way that the final images can be viewed and analyzed in the same coordinate system. Image registration is classified as being "rigid" or "non-rigid". The rigid technique allows only a global change on the image, whereas the non-rigid technique allows also local changes, without necessarily changing the image as a whole(9–13). The results described in the present study are associated with the utilization of rigid image registration, only by a geometry-based approach without deformation. The reliability of the anatomical identification tends to improve with the utilization of the rigid technique, but significant limitations may be observed in situations where the patient presents a marked anatomical variation such as, for example, presence of artifacts on images of patients with a marked ventricular dilatation. The most recent techniques based on voxels similarity measurements utilize comparison between voxels intensity on source- and target-images to define transformation parameters with the advantage of being completely automated, differently from the previous techniques based on objects recognition which depended on preliminary marking and/or segmentation steps. Some measurements can be utilized by registration algorithms for calculation of image voxels similarity, namely, cross-correlation measurements and information theory measurements. The crosscorrelation measurement technique presents better results in cases where there is a linear relationship between intensities on the images to be aligned, and most frequently is utilized for intramodality registration. On the other hand, for intermodality registration (images acquired through different techniques) where the relationship between voxels intensities is non-linear, information theory measurements, particularly mutual information and normalized mutual information, are most frequently utilized(9–13). Image registration techniques based on voxels similarity through correlation measurements are considered as the ideal techniques for template images construction and other activities requiring alignment of images from a same modality(9–13). In the present study, the authors utilized the cross correlation measurement, a normalized correlation coefficient version for images registration. Considering that all myocardial perfusion scintigraphy images present a same spatial disposition, voxel-by-voxel mathematical operations can be performed, resulting in reliable images reflecting such operations. So, with images normalized according to a 100-level gray-scale for ten individuals of each gender with low probability of coronary artery disease and considered as normal by two experienced observers, the authors obtained template images corresponding to mean and standard deviation for perfusion uptake for a myocardium considered as normal for both male and female patients under physiological stress/rest conditions. Images from one male and one female testpatients, also normalized according to a 100-level gray-scale and with reports of two specialists indicating ischemic cardiopathy, were statistically compared with templates images created by means of a computational algorithm. The final results corresponded to images whose overlapping with test-patients images indicate the presence of regions with a probable myocardial perfusion defect. Also, it is important to note that the regions with perfusion defects are visualized on tomographic sections through the described algorithm, contrarily to the classical visualization through polar maps, which makes the human observation process more intuitive. A similar approach has been described by Slomka et al.(7), who have created normality template images based on images of 23 men and 15 women, which were later utilized for quantifying perfusional abnormalities in test-patients. For image registration, these authors have developed and tested a hybrid image registration algorithm based on principal-axes transformation and minimization technique. The present study is differentiated by the utilization of images registration based on correlation measurements classically accepted as ideal for intramodality medical images registration and template images construction(9–13), besides the utilization of image templates, statistical measurements and images processing techniques for automatic detection and definition of regions of probable perfusion defect on SPECT sections of patients with ischemic cardiopathy aiming at offering the observer a "second diagnostic opinion". Although the initial results of the present study have demonstrated the potential of the method proposed based on the agreement about the defect regions automatically detected by means of a visual analysis by two experienced observers, it should be observed that, certainly, the criteria for selection of normal cases, as well their number and processing method utilized for creating the template images, are certainly not sufficient for validating the method. However, the proposal of the present study, in the current phase, was to prove the concept validity, so justifying further detailed investigation with a more representative number of cases, including comparison with a quantitative golden-standard to evaluate the sensitivity and specificity that could be achieved in actual clinical situations.
CONCLUSION The techniques for images processing utilized in the present study have shown to be effective for the development of the atlas of SPECT myocardial perfusion scintigraphy. However, further techniques should be evaluated, applied and compared for development of new template images, besides a more clear-sighted selection of normal cases to enhance the reliability of the atlas. As a proof of concept, the method proposed for comparing patients' images with the atlas image templates has shown to be promising as an aid in the detection of myocardial perfusion defects on SPECT images. Future refinements in the algorithm and quantitative experiments with a higher number of patients, besides the inclusion of control cases, are required for evaluation of the sensitivity/specificity and validation of the method.
REFERENCES 1. Azevedo-Maques PM. Diagnóstico auxiliado por computador na radiologia. Radiol Bras. 2001;34: 285–93. [ ] 2. Doi K. Computer-aided diagnosis in medical imaging: historical review, current status and future potential. Comput Med Imaging Graph. 2007;31: 198–211. [ ] 3. Cullom SJ. Principles of cardiac SPECT. In: DePuey EG, Garcia EV, Berman DS, editors. Cardiac SPECT imaging. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 3–14. [ ] 4. Yoo TS. Introduction. In: Yoo TS, editor. Insight into images: principles and practice for segmentation, registration, and image analysis. Wellesey: AK Peters; 2004. p. 3–17. [ ] 5. Hendel RC, Corbett JR, Cullom SJ, et al. The value and practice of attenuation correction for myocardial perfusion SPECT imaging: a joint position statement from the American Society of Nuclear Cardiology and the Society of Nuclear Medicine. J Nucl Med. 2002;43:273–80. [ ] 6. Van Train KF, Garcia EV, Cooke CD, et al. Quantitative analysis of SPECT myocardial perfusion. In: DePuey EG, Garcia EV, Berman DS, editors. Cardiac SPECT imaging. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 41–64. [ ] 7. Slomka PJ, Hurwitz GA, Stephenson J, et al. Automated alignment and sizing of myocardial stress and rest scans to three-dimensional normal templates using an image registration algorithm. J Nucl Med. 1995;36:1115–22. [ ] 8. Itti E, Klein G, Rosso J, et al. Assessment of myocardial reperfusion after myocardial infarction using automatic 3-dimensional quantification and template matching. J Nucl Med. 2004;45:1981–8. [ ] 9. Hajnal JV, Hill DLG, Hawkes DJ. Medical image registration. Boca Raton: CRC Press; 2001. [ ] 10. Ng L, Ibanez L. Medical image registration: concepts and implementation. In: Yoo TS, editor. Insight into images: principles and practice for segmentation, registration, and image analysis. Wellesey: AK Peters; 2004. p. 239–95. [ ] 11. Zitová B, Flusser J. Image registration methods: a survey. Image and Vision Computing. 2003; 21:977–1000. [ ] 12. Oliveira LF, Azevedo-Marques PM, Wichert-Ana L, et al. Support software for clinical diagnosis in epilepsy: B.R.A.S.I.L. brain registration and subtraction: improved localization for SPECT analysis. Int J Comput Assist Radiol Surg. 2006; (1 Suppl 1):386–9. [ ] 13. Mäkelä T, Clarysse P, Sipilä O, et al. A review of cardiac image registration methods. IEEE Trans Med Imag. 2002;21:1011–21. [ ] 14. Hartkens T, Rueckert D, Schnabel JA, et al. VTK CISG registration toolkit: an open source software package for affine and nonrigid registration of single- and multimodal 3D images. Bildverarbeitung für die Medizin. 2002:409–12. [ ] 15. Schroeder W, Martin K, Lorensen B. The visualization toolkit: an object-oriented approach to 3D graphics. 4th ed. Clifton Park: Kitware; 2006. [ ] 16. Kitware, Inc. The VTK user's guide: install, use and extend the visualization toolkit. 5th ed. Clifton Park: Kitware; 2006. [ ] Received September 14, 2008. Accepted after revision November 6, 2008. * Study developed in the Division of Cardiology and Unit of Nuclear Medicine at Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554