Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 5 - Sep. / Oct. of 2008
Vol. 41 nº 5 - Sep. / Oct. of 2008
|
CASE REPORT
|
|
Leiomyomatosis peritonealis disseminata: a case report |
|
|
Autho(rs): Marco Antonio Marini Gedda, Giuliano Arrivabeni Piantavinha, Túlio Rebello Coutinho, Silvana Machado Mendonça, Gustavo de Vasconcelos Bello |
|
|
Keywords: Leiomyomatosis peritonealis disseminata, Oral contraceptive method, Computed tomography, Magnetic resonance imaging |
|
|
Abstract:
Marco Antonio Marini Gedda; Giuliano Arrivabeni Piantavinha; Túlio Rebello Coutinho; Silvana Machado Mendonça; Gustavo de Vasconcelos Bello MDs, Residents in Radiology and Imaging Diagnosis at Clínica Radiológica Emílio Amorim, Rio de Janeiro, RJ, Brazil
INTRODUCTION Few cases of leiomyomatosis peritonealis disseminata have been reported in the literature, but there is a possibility that the incidence of this disease may be higher, considering that many patients are asymptomatic and the finding of the disease ends up being incidental(1). Usually, this is a benign condition affecting women in childbearing age, and is generally associated with pregnancy or utilization of oral contraceptive methods. It is suspected that this disease originates from a metaplasia of submesothelial multipotent mesenchymal cells(2). Some authors suggest that exposure to estrogen is the primary mechanism in the development of this disease and, frequently, this condition is associated with the presence of uterine fibroids(3,4). In the present article, the authors present a case of leiomyomatosis peritonealis disseminata in a patient who presented with periumbilical swelling and diffuse abdominal pain.
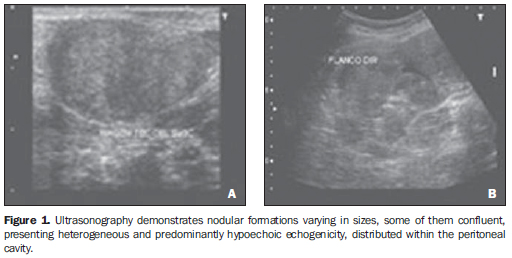
CASE REPORT A female, 46-year-old patient born in São Gonçalo dos Campos, BA, Brazil, where she lived up to her 18 years of age when she moved to Rio de Janeiro. The patient was single, housewife who complained of the presence of a mass in her umbilicus during the premenstrual period. The patient reported that three years ago she had observed a mild periumbilical swelling appearing invariably in the premenstrual period, generally 7 to 15 days before the first day of menstruation. Concomitantly, the patient reported an initially diffuse mild abdominal pain, progressively becoming localized in the right iliac fossa. The pain disappeared at the first day of menstruation and the periumbilical swelling decreased in the following days, although without disappearing completely. Two years ago, she had undergone ultrasonography (US) in a public health service and, as reported, uterine myomatosis had been found. Her clinical picture had remained stable up to three months ago, when she went to another health unit, undergoing a new US scan that, again, as reported, demonstrated uterine fibroids. Oral contraceptives were prescribed, but no improvement was observed. Then, the patient was referred to our institution to be submitted to computed tomography (CT) and magnetic resonance imaging (MRI). Eight years ago, the patient had been submitted to myomectomy, when four uterine fibroids were removed. She reported hypertension being treated with hydrochlorotiazide and atenolol for three years and had already utilized oral contraceptives between her 18 and 37 years of age. Gynecologic history: GII, P0, AII (both by curettage), menarche at 16 years of age and regular menstrual cycles at 29-day intervals. At clinical examination, the patient presented abdominal distention with the abdomen depressable upon superficial or deep palpation, with reflex and diffuse pain most intensely observed in the right iliac fossa. A median inferior surgical scar and a bulging, poorly defined, palpable mass occupying a great part of the lower abdomen were observed. Dullness to percussion was observed in the periumbilical region as well as in the lower abdomen. Painful cul-de-sac under two-handed palpation. Nodular formations, some of them confluent, were observed at US (Figure 1) with intermediate echogenicity and hypoechoic areas. The lesions were intermingled with loops, protruding through the umbilical region, filling the pelvis and attached to the uterus. Increased uterine volume was observed with the presence of myomatous nodules.
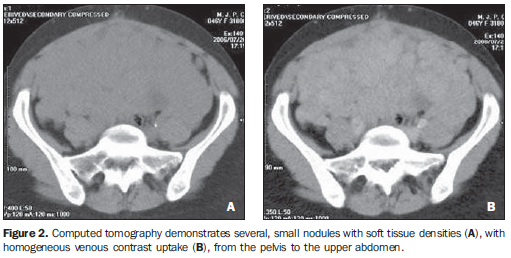
At CT, innumerable nodules with soft tissues density and varying in size were observed within the abdominal cavity from the pelvis to the upper abdomen. The nodules demonstrated homogeneous contrast uptake. In the pelvis, confluent nodules formed a mass with possible central necrosis. No sign of ureteral and rectal invasion was observed despite the involvement of these structures (Figure 2).
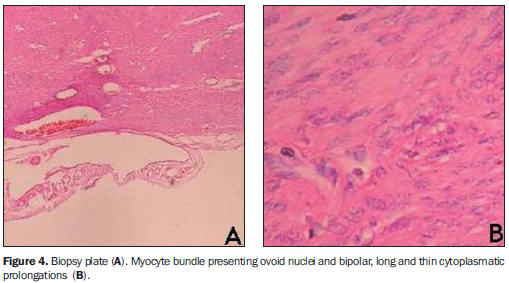
The nodular characteristic of the lesion as well as its localization in the mesenterium and omentum were most easily observed at MRI. On non-contrast enhanced T1-weighted sequences, the lesions were isointense to the muscle, with lower intensity in the center. Contrast-enhancement was observed and the hyposignal remained unchanged in the center of the mass. On T2-weighted images, heterogeneous signal intensity was observed with predominance of hypersignal (Figure 3). The definite diagnosis was achieved with a biopsy of abdominal nodule (Figure 4).
DISCUSSION Leiomyomatosis peritonealis disseminata is a rare disease, with a little more than 100 cases reported. Most of times, the patients are asymptomatic, and the disease is incidentally found, so there is a possibility that the disease incidence is higher than the number of cases described in the literature(1). The disease etiology still remains unknown. It is suspected that this disease originates from a metaplasia of submesothelial multipotent mesenchymal cells(2). Apparently, this is not a familial or inherited disease, despite the case of several members of a same family affected by leiomyomatosis peritonealis disseminata(5). Although 10% of cases may present malignant degeneration, this is usually a benign condition, characterized by the presence of multiple smooth-muscle nodules in the peritoneal surface, affecting women in childbearing age. It is generally associated with pregnancy or utilization of oral contraceptive methods(1,2,4). According to some authors, exposure to estrogen is the primary mechanism involved in the development of leiomyomatosis peritonealis disseminata(3,4). Two cases have been reported associating the disease with the utilization of tamoxifen for the management of breast cancer(6,7). There are cases of leiomyomatosis peritonealis regression after delivery or suspension of oral contraceptive methods(4,8). Post-treatment recurrence is rarely reported. This condition is frequently associated with uterine fibroids. On the other hand, association with endometriosis is not frequent. Sometimes the imaging diagnosis may be difficult, considering that radiological findings may suggest the presence of a malignant condition(3,9). At US, the present case showed small, clustered nodules in the lower abdomen and pelvis, simulating a lobulated mass and presenting a variable echogenicity, with apparently cystic areas inside. At CT (Figure 1) and MRI (Figures 2 and 3) a confluent nodular pattern was observed, with soft tissues density, seeming a single mass. No sign of ureteral invasion was found. Some of the nodules presented areas of cystic degeneration.
CONCLUSION The patient whose case is reported in the present study was within the age range expected for this disease and presented a history of chronic exposure to estrogen that is characteristically reported in most of recorded cases. Additionally, imaging findings were compatible with those described the literature, demonstrating confluent nodules seeming a single mass with homogeneous contrast uptake both at CT and MRI. Acknowledgements The authors thank Dr. Marília Magalhães, Dr. Rosangela Guerreiro, Dr. Euniro de Macedo Melo, Dr. Leila Freitas, Dr. Carlos Peixoto and Dr. Arno Von Ristow, for their cooperation along the development of the present study.
REFERENCES 1. Borsellino G, Zante P, Ciraldo MC. Diffuse peritoneal leiomyomatosis. A clinical case report. Minerva Ginecol. 1997;49:53-7. [ ] 2. Abulafia O, Angel C, Sherer DM, et al. Computed tomography of leiomyomatosis peritonealis disseminata with malignant transformation. Am J Obstet Gynecol. 1993;169:52-4. [ ] 3. Sobiczewski P, Bidziński M, Radziszewski J, et al. Disseminated peritoneal leiomyomatosis - case report and literature review. Ginekol Pol. 2004;75:215-20. [ ] 4. Bekkers RL, Willemsen WN, Schijf CP, et al. Leiomyomatosis peritonealis disseminata: does malignant transformation occur? A literature review. Gynecol Oncol. 1999;75:158-63. [ ] 5. Halama N, Grauling-Halama SA, Daboul I. Familial clustering of leiomyomatosis peritonealis disseminata: an unknown genetic syndrome? BMC Gastroenterol. 2005;5:33. [ ] 6. Danikas D, Goudas VT, Rao CV, et al. Luteinizing hormone receptor expression in leiomyomatosis peritonealis disseminata. Obstet Gynecol. 2000;95(6 Pt 2):1009-11. [ ] 7. Lubczyk V, du Bois A, Fisseler-Eckhoff A. Leiomyomatosis peritonealis disseminata and borderline lesion. Pathologe. 2005;26:291-5. [ ] 8. Bristow RE, Montz FJ. Leiomyomatosis peritonealis disseminata and ovarian Brenner tumor associated with tamoxifen use. Int J Gynecol Cancer. 2001;11:312-5. [ ] 9. Cohen DT, Oliva E, Hahn PF, et al. Uterine smooth-muscle tumors with unusual growth patterns: imaging with pathologic correlation. AJR Am J Roentgenol. 2007;188:246-55. [ ] Received March 27, 2007. Accepted after revision June 14, 2007. * Study developed at Clínica Radiológica Emílio Amorim, Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554