Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 5 - Sep. / Oct. of 2008
Vol. 41 nº 5 - Sep. / Oct. of 2008
|
REVIEW ARTICLE
|
|
Magnetic resonance imaging and computed tomography of the temporomandibular joint: beyond dysfunction |
|
|
Autho(rs): Marcelo de Mattos Garcia, Karina Freitas Soares Machado, Marcelo Henrique Mascarenhas |
|
|
Keywords: Temporomandibular joint, Computed tomography, Magnetic resonance imaging |
|
|
Abstract:
ITitular Members of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MDs, Radiologists at Clínica Axial Centro de Imagem, Belo Horizonte, MG, Brazil
INTRODUCTION The most prevalent alteration involving temporomandibular joints (TMJs) is internal derangement(1). This term refers to an abnormal disk positioning and inappropriate functional relationship between the disk and articular surfaces. Pain, clicking and restricted functionality constitute frequent complaints among patients affected by this dysfunction. However, this clinical picture is quite non-specific and several other non-dysfunctional diseases, conditions not directly localized in these joints included, may be responsible for symptoms reported by the patients(2). Not rarely, non-dysfunctional diseases such as arthritis and expansile lesions, among others, are initially confused with internal derangement, delaying the definitive diagnosis and consequently the adoption of an appropriate management. Like in the evaluation of dysfunctional conditions, computed tomography (CT) and magnetic resonance imaging (MRI) are quite useful in the assessment of these patients, with higher accuracy than conventional radiographic studies. The advent of the multislice technology has significantly improved the images acquisition time, besides allowing high-quality multiplanar images acquisition because of the isotropic acquisition properties of the method(3). The high-resolution of the method is ideal for assessing bone structures and their abnormalities. Currently, a 16-channel multislice CT equipment is utilized for 0.75 mm collimation volume acquisitions, with open and closed mouth views. Later, images are analyzed on the axial, coronal and sagittal planes, and the volume rendering technique is utilized for 3D images reconstruction. MRI is currently the method of choice for evaluating this joint, because of its excellent capability to demonstrate the TMJ anatomy, particularly when a specific surface coil is employed(1). High contrast resolution images demonstrate soft tissues and can be obtained with the mouth closed or at different degrees of mouth opening, therefore providing functional data. In the author's institution, the protocol described on Table 1 is utilized, and the utilization of intravenous paramagnetic contrast agent is reserved for cases where an evaluation of a possible inflammatory process is required. The present study sought to demonstrate by means of CT and MRI, different non-dysfunctional lesions of the TMJ, highlighting the significance of these pathological conditions in the differential diagnosis for patients with complaints regarding these joints.
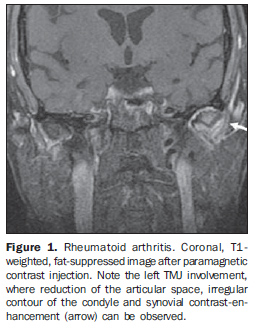
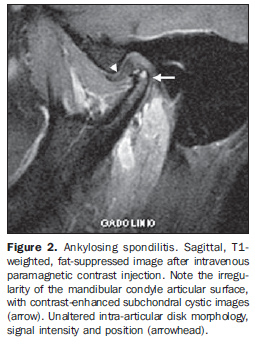
ARTHRITIS Different inflammatory processes may affect the TMJ, usually characterized by edema and synovial proliferation, such as retrodiskitis, rheumatoid arthritis, ankylosing spondilitis, psoriatic arthritis, systemic lupus erythematosus and juvenile rheumatoid arthritis(4). Both the pathophysiology of these conditions as well as the patients' clinical complaints are similar(5). Generally, symptoms correspond to pain during the active phase of the disease, limited mouth opening, morning rigidity and crepitation as result of secondary osteoarthritis. Clicking, however, is not a frequent symptom. Imaging studies can demonstrate the presence of cortical erosion and signs of secondary osteoarthritis, ankylosis at terminal stages of the disease included. Bone alterations can be better characterized by CT. In the active phase of the disease, articular effusion, bone marrow edema and synovial contrast-enhancement can be better visualized by MRI (Figure 1), corresponding to the presence of pannus. The contrast-enhancement, however, is non-specific and does not allow the differentiation between primary inflammation and osteoarthritis(5). Similarly, there is no significant difference in the imaging findings of the different inflammatory processes that may involve this joint (Figure 2). Granulation and pannus formation, like in other joints, typically occur in naked areas of cartilage adjacent to capsular insertions.
A recent study utilizing technetium-99m-labeled leukocyte in an animal model has demonstrated that this scintigraphic method can early and accurately identify an inflammatory process before structural alterations have developed(6).
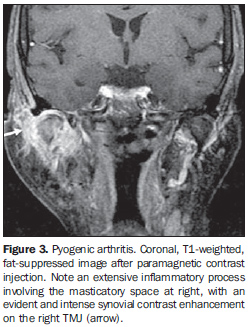
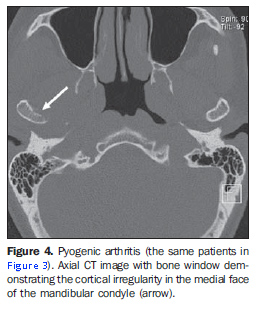
INFECTION Granulomatous or pyogenic infections are uncommon, and may occur as a result of hematogenic dissemination of a distant infection or, most frequently, as a result of a direct extension of an oral infection or following TMJ surgeries(4). Radiological findings are similar to the ones described for arthritis in general(4), with evident intra-articular effusion, thickening and synovial contrast-enhancement (Figure 3), which are better characterized at MRI. Subtle bone irregularities can be better detected by computed tomography (Figure 4). The clinical progression of the disease is rapid, and the clinical history and physical examination are quite characteristic, considering that local increase in volume can be observed as a result of edema and intra-articular effusion. Usually, intense local pain and marked functional limitation are observed.
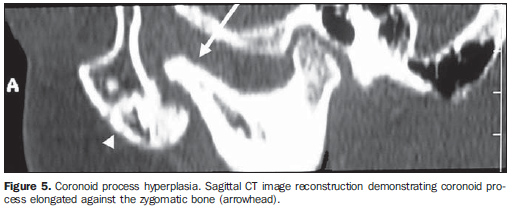
CORONOID PROCESS HYPERPLASIA Coronoid process hyperplasia is a generally unpainful disorder characterized by restricted jaw movement. The cause for this condition is still to be determined, and both unilateral(7) and bilateral(8) presentations are reported in the literature. In these cases, the coronoid process elongates at least 1 cm above the lower border of the zygomatic arch with possible impingement on the zygomatic bone (Figure 5) of the maxilla, where frequently the presence of bone remodeling and sclerosis is observed. These alterations can be detected by conventional radiography, but CT is more effective for characterizing morphological alterations as well as alterations secondary to the impingement of the hyperplasied coronoid process against the zygomatic bone and the proximal contiguous segment of the zygomatic arch(9). Considering that this condition is poorly known by radiologists, and its occurrence may be underestimated(10). Generally, the surgical management with coronoid process resection is successful.
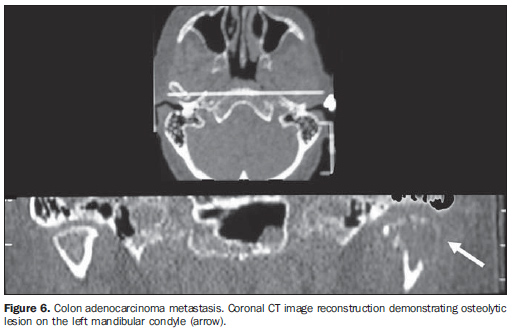
SECONDARY NEOPLASTIC PROCESS Metastases to the TMJ are not frequent, but this hypothesis should not be disregarded in the differential diagnosis of painful syndromes affecting this region. Most frequently, secondary lesions arising from adenocarcinomas (Figure 6) affect the mandible. In order of frequency, metastases from primary lesions in the breasts, kidneys, lungs, colon, prostate, thyroid, stomach, skin and testicles may affect this region(11). Lesions are most frequently found in the molar and premolar regions, with involvement of the mandibular condyle being less frequent. Computed tomography can demonstrate the presence of lytic or blastic bone lesions, depending on the nature of the primary lesion(12). MRI, however, presents a higher resolution for demonstrating soft tissue components and respective extent, particularly on T1-weighted, fat-suppressed sequences after intravenous paramagnetic contrast agent injection.
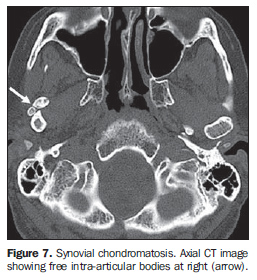
SYNOVIAL CHONDROMATOSIS Synovial chondromatosis is characterized by a cartilaginous metaplasia in the synovial membrane producing small cartilage nodules that can break off from the synovial membrane. These fragments may be found freely within the joint cavity and eventually calcify. Rarely this condition affects the TMJ, but, generally, cases where this joint is involved affect patients in their fourth and fifth decade of life, and most frequently involve women(13). Symptoms reported by patients are vague, and usually their complaints are related to pain and swelling in the region, with facial asymmetry and occlusal problems included. CT studies demonstrate the presence of generally multiple intra-articular calcified bodies (Figure 7). The mandibular condyles may be preserved or with signs of osteoarthritis, with irregularities on the joint surface being observed(14). In cases where a higher aggressiveness is observed, destruction of the condyle and articular fossa may be found, with intracranial extension included, as already reported(15,16).
MRI can demonstrate the presence of intra-articular effusion, signs of paramagnetic contrast-enhanced synovitis, and presence of intra-articular masses with heterogeneous signal, generally, with hyperintensity on T2-weighted sequences(12), which may be located within the upper as well as in the lower compartments of the joint, and also posteriorly to the mandibular condyle. Calcified lesions present with hypointense signal on T1- and T2-weighted images(14), especially on gradient-echo sequences.
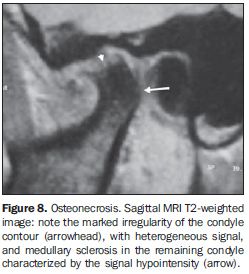
OSTEONECROSIS Avascular necrosis of the mandibular condyle corresponds to an area with cortical and medullary infarction, resulting in structural weakening that predisposes to collapse and degenerative alterations(17). This condition may be associated with hematological disorders, bone dysplasia, chemotherapy, corticosteroid therapy, trauma, or occurring as a result of orthognatic surgery complications(18). However, the majority of cases are related to advanced stages of internal derangement of the TMJ(18). Pain is the predominant symptom, and may be constant, sometimes reported as pulsatile, exacerbated by the articular movement. Other frequent complaints include headache, otalgia, masticatory muscle spasm and pain, limited mouth opening and crepitation. Radiographic and tomographic findings include asymmetric condylar morphology, focal defects and depression on the articular surface of the condyle, besides decrease in the condylar volume (Figure 8).
MRI is quite sensitive in the diagnosis of osteonecrosis(17) and, besides morphological alterations, can demonstrate the presence of altered signal intensity in the condylar bone marrow. This alteration is characterized by signal hypointensity on T1-weighted sequences, and variability in signal intensity on T2-weighted sequences (Figure 8), depending on the phase where the study is performed. In a earlier stage, signal hyperintensity can be observed on T2-weighted sequences, corresponding to the presence of edema resulting from vascular congestion. On the other hand, at the later phases of the process, signal hypointensity can be observed on T2-weighted sequences, corresponding to medullary replacement by fibrotic tissue and bone sclerosis. However, it should be highlighted that these alterations are not pathognomonic of avascular necrosis, and MRI does not allow rule out the hypothesis of medullary fibrosis not resulting from osteonecrosis(11). Additionally, histological evidences may demonstrate the presence of edema, with no evidence of osteonecrosis, or as a possible precedent factor(19).
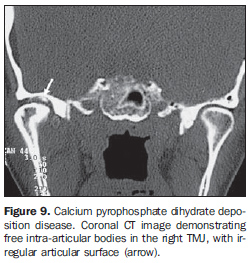
CALCIUM PYROPHOSPHATE DIHYDRATE DEPOSITION DISEASE (PSEUDOGOUT) Metabolic arthritis rarely affects the TMJs. Most frequently this condition affects women with > 40 years of age. The pathophysiology of the disease is still to be completely known. Crystals of calcium pyrophosphate dehydrate must originate from articular chondrocytes and their release would occur because of a mechanism of reparation of cartilaginous surface lesions. Therefore, the level of these crystals may be high in the synovial fluid of the affected joint, and normal in the blood and urine of these patients(13). The clinical picture is generally characterized by acute onset of pain, with local pain and edema. Imaging studies can demonstrate the presence of gross or subtle intra-articular calcifications, the subtle ones being more easily detected by CT (Figure 9). Erosion may be found both in the mandibular condyle and in the articular fossa; however, late detection of the corresponding radiological alterations may occur in cases of few, sparse crisis episodes along an extensive period of time(20).
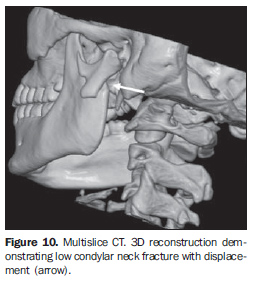
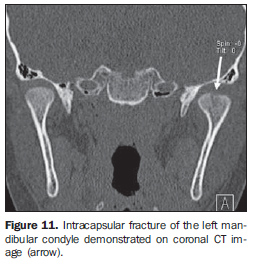
TRAUMA The prevalence of condylar process fractures corresponds to 25%-50% of all mandibular fractures, the condylar/subcondylar region being the most frequently fractured portion of the mandible. These fractures can be classified as condylar neck fractures and condylar head fractures. Condylar neck fractures can be high, medium or low (Figure 10), depending on their positioning. On the other hand, condylar head fractures can be subdivided into intracapsular (Figure 11) and extracapsular(5).
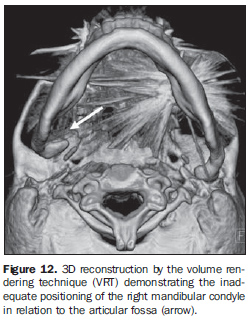
Intracapsular fractures are less common and, most frequently affect children. Extracapsular fractures involve the subcondylar region and most frequently occur unilaterally, eventually in association with contralateral mandibular angle fracture(21). The differentiation between high condylar neck fracture and extracapsular condylar head fracture is somewhat arbitrary. Condylar process fractures can further be subdivided into displaced and nondisplaced fractures. Typically, because of the traction exerted by the pterygoid muscle, fractures are medially displaced. The evaluation of the type and degree of disk displacement is critical for the therapeutic planning, considering the angle between the mandibular head and ramus, the contact between the fracture ends (particularly the degree of contraction in the vertical plane that affects the occlusion), the transverse displacement, and the position of the fractured head as related to the articular eminence and articular fossa, these parameters being useful in the decision making about a surgical or non-surgical approach(5). Generally, the initial evaluation is performed by means of conventional radiography, particularly panoramic radiography of the mandible, because of the low expensiveness, high availability and experience with the method. CT is considered as the imaging method of choice for evaluating facial traumas. The multislice technology has considerably reduced the CT images acquisition time, achieving an improved coverage of the sample volume, besides allowing imaging of different high-resolution angles and planes, and excellent 3D images reconstruction, constituting a quite useful tool in the planning of reconstructive surgeries(21). MRI can be useful in the identification of post-traumatic disk displacement, as well as capsular, cartilaginous and ligamentous lesions, playing a significant role in the pretreatment evaluation of condylar process fractures. The treatment is aimed at an appropriate reduction and consolidation of the fracture, preservation of the dental occlusion and articular function, besides a good aesthetic outcome. Functional disorders, dental maloccusion, pseudoarthrosis, pain, ankylosis and osteoarthritis constitute complications of inappropriate fracture consolidation(5) (Figure 12).
The selection of open or closed reduction techniques depends on the injury type and severity, presence of unilateral or bilateral fracture, as well as the patient's age and comorbidities. Generally, the conservative treatment is preferred in cases of unilateral or bilateral nondisplaced fractures in children. The surgical management is reserved for cases of displaced fractures, even the unilateral ones, provided the articular movement amplitude is impaired or dental malocclusion is present.
CONCLUSIONS Internal derangement corresponds to the main pathologic entity found in patients with TMJ-related complaints. Pain, clicking and functional limitation predominate in the clinical picture. However these signs and symptoms are non-specific and may be found in several non-dysfunctional conditions, including inflammatory processes, expansile lesions and post-traumatic alterations, among others. Imaging methods are quite useful in the diagnosis of these conditions which frequently are not considered as primary clinical suspicion. MRI and CT present a higher diagnostic accuracy as compared with conventional radiology, considering their higher anatomical resolution. CT is ideal for evaluating bone structures, while MRI allows the evaluation of soft tissues, the intra-articular disk included. Frequently, these methods are complementary in the study of the TMJ abnormalities, playing a relevant role in the differential diagnosis of several conditions affecting this region. Additionally, other studies demonstrate that differentiated and symmetrical morphological alterations of the styloid process radiographically evaluated in patients with temporomandibular joints disorder occur independently from gender and age(22).
REFERENCES 1. Rao VM, Bacelar MT. MR imaging of the temporomandibular joint. Magn Reson Imaging Clin N Am. 2002;10:615-30. [ ] 2. Heo MS, An BM, Lee SS, et al. Use of advanced imaging modalities for the differential diagnosis of pathoses mimicking temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:630-8. [ ] 3. Dalrymple NC, Prasad SR, El-Merhi FM, et al. Price of isotropy in multidetector CT. Radiographics. 2007;27:49-62. [ ] 4. Murphy WA, Kaplan PA. Temporomandibular joint. In: Resnick D, editor. Diagnosis of bone and joint disorders. Philadelphia: Saunders; 1995. p. 1699-754. [ ] 5. Sommer OJ, Aigner F, Rudisch A, et al. Cross-sectional and functional imaging of the temporomandibular joint: radiology, pathology and basic biomechanics of the jaw. Radiographics. 2003;23: e14. Epub 2003 Aug 14. [ ] 6. Brasileiro CB, Cardoso VN, Ruckert B, et al. Avaliação de processos inflamatórios na articulação temporomandibular empregando leucócitos autólogos marcados com tecnécio-99m em modelo animal. Radiol Bras. 2006;39:283-6. [ ] 7. Lucaya J, Herrera M, Vera J. Unilateral hyperplasia of the coronoid process in a child: a cause of restricted opening of the mouth. Radiology. 1982;144:528. [ ] 8. Kreutz RW, Sanders B. Bilateral coronoid hyperplasia resulting in severe limitation of mandibular movement: report of a case. Oral Surg Oral Med Oral Pathol. 1985;60:482-4. [ ] 9. Munk PL, Helms CA. Coronoid process hyperplasia: CT studies. Radiology. 1989;171:783-4. [ ] 10. Isberg A, Isacsson G, Nah KS. Mandibular coronoid process locking: a prospective study of frequency and association with internal derangement of the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1987;63:275-9. [ ] 11. Westesson PL, Yamamoto M, Sano T, et al. Temporomandibular joint. In: Som P, Curtin HD, editors. Head and neck imaging. St Louis: Mosby; 2003. p. 995-1053. [ ] 12. Larheim TA, Westesson PL. Temporomandibular joint. In: Larheim TA, Westesson PL, editors. Maxillofacial imaging. Berlin, Heidelberg, New York: Springer; 2006. p. 143-78. [ ] 13. Fernandes JL, Viana SL. Avaliação por imagem das artropatias por deposição de cristais. In: Fernandes JL, Viana SL. Diagnóstico por imagem em reumatologia. Rio de Janeiro: Guanabara Koogan; 2007. p. 178-204. [ ] 14. Heffez LB. Imaging of internal derangements and synovial chondromatosis of the temporomandibular joint. Radiol Clin North Am. 1993;31:149-62. [ ] 15. Quinn PD, Stanton DC, Foote JW. Synovial chondromatosis with cranial extension. Oral Surg Oral Med Oral Pathol. 1992;73:398-402. [ ] 16. Sun S, Helmy E, Bays R. Synovial chondromatosis with intracranial extension. A case report. Oral Surg Oral Med Oral Pathol. 1990;70:5-9. [ ] 17. Gillespy T 3rd, Genant HK, Helms CA. Magnetic resonance imaging of osteonecrosis. Radiol Clin North Am. 1986;24:193-208. [ ] 18. Schellhas KP, Wilkes CH, Fritts HM, et al. MR of osteochondritis dissecans and avascular necrosis of the mandibular condyle. AJR Am J Roentgenol. 1989;152:551-60. [ ] 19. Larheim TA, Westesson PL, Hicks DG, et al. Osteonecrosis of the temporomandibular joint: correlation of magnetic resonance imaging and histology. J Oral Maxillofac Surg. 1999;57:888-98. [ ] 20. Laskin DM. Diagnosis of pathology of the temporomandibular joint. Clinical and imaging perspectives. Radiol Clin N Am. 1993;31:135-47. [ ] 21. Cinnamon J, Shanmuganathan K, Robertson BC. Computed tomography of maxillofacial trauma: patterns of osseous injury and associated soft tissue involvement. In: Mirvis SE, Shanmuganathan K, editors. Imaging in trauma and critical care. Philadelphia: Saunders; 2003. p. 133-83. [ ] 22. Guimarães SMR, Carvalho ACP, Guimarães JP, et al. Prevalência de alteração morfológica do processo estilóide em pacientes com desordem temporomandibular. Radiol Bras. 2006;39:407-11. [ ] Received September 17, 2007. Accepted after revision January 8, 2008. * Study developed at Clínica Axial Centro de Imagem, Belo Horizonte, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554