Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 4 - July / Aug. of 2008
Vol. 41 nº 4 - July / Aug. of 2008
|
CASE REPORT
|
|
Degenerating cystic uterine fibroid mimics an ovarian cyst in a pregnant patient: a case report |
|
|
Autho(rs): Arildo Corrêa Teixeira, Linei A. B. D. Urban, Mauricio Zapparoli, Caroline Pereira, Thaís Cristina Cleto Millani, Ana Paula Passos |
|
|
Keywords: Ultrasonography, Magnetic resonance imaging, Leiomyoma |
|
|
Abstract:
IProfessor of Gynecology and Obstetrics at Hospital de Clínicas da Universidade Federal do Paraná (UFPR), Curitiba, PR, Brazil
INTRODUCTION Uterine leiomyomas are the most frequently found benign solid tumors of the female genital system. These tumors affect 20% to 30% of women at childbearing age, and more than 40% of women above 40 years of age(1,2). Leiomyomas are estrogen-dependent tumors presenting growth during gestation in up to 50% of cases(3). Initially, ultrasonography (US) is the method of choice for evaluating these lesions. Leiomyomas have a typical appearance, but variations in presentation occur as a result from degenerative factors such as hemorrhage, hyalinization and myxoid degeneration mimicking other diseases(2,4). Magnetic resonance imaging (MRI) has shown to be a valuable tool in the diagnosis of these cases(2,5). The authors present the case of a subserosal fibroid with cystic degeneration mimicking an adnexal neoplasm in a primigravida.
CASE REPORT A 28-year-old, asymptomatic primigravida referred to the institution presenting a complex mass in the right iliac fossa demonstrated at a second-trimester ultrasonography. A new US demonstrated a single fetus with biometric data corresponding to a 20/21-week gestation. A large, mixed, predominantly cystic lesion was observed in the right adnexal region, presenting a thick content, irregular septa and peripheral flow, with 662 cm³ in volume, suggesting an ovarian neoplasm (Figure 1).
MRI for preoperative evaluation demonstrated a gravid uterus, with small intramural and subserosal fibroids. Additionally, a complex cystic formation was observed in the iliac fossa, suggesting a degenerating subserosal fibroid, considering that the lesion was involved by the uterine serosa. The ovaries could not be visualized (Figure 2).
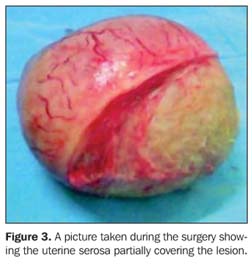
The patient was submitted to laparotomy, with a surgical finding of a large, pedunculated subserosal fibroid in the right cornual region. A complete enucleation was performed, with no intercurrence (Figure 3). Histopathological study confirmed the diagnosis of degenerating leiomyoma.
DISCUSSION Leiomyomas are predominantly composed of smooth muscle cells surrounded by a pseudocapsule(2,4). Leiomyomas may often enlarge during pregnancy or oral contraceptive use, besides regressing at the climacteric and puerperal periods(2). Enlargement during the gestational period presents a multifactorial etiology, and may be related to myometrial hypertrophy, higher vascularization and changes in the local steroid receptors. As leiomyomas enlarge, an imbalance between oxygen demand and supply is observed, causing areas of degeneration(2). Among the degeneration types observed during gestation, the benign ones are most frequently found, particularly the hyaline, myxoid, red and cystic degenerations. Malignant sarcomatous degeneration is observed in only 0.5% of fibroids, and whether malignancy is primary or secondary to degeneration is still controversial(3). Pelvic US is initially the method of choice for assessing leiomyomas(1). Besides evaluating the gestation, first-trimester US may demonstrate the presence of fibroids as well as following up their progression. Typically, leiomyomas present as hypoechoic, circumscribed, homogeneous nodules localized in the submucosal, intramural or subserosal region of the uterine body and, less frequently, of the uterine cervix(3). Frequently, the diagnosis of degenerating fibroids is difficult, because of the heterogeneity in their presentation. Cystic degeneration generally manifests as a lesion with irregular walls, presenting cystic areas with solid contents(3). In the present case, US suggested the diagnosis of an ovarian neoplasm as a function of the presence of a predominantly cystic, unilocular, thin-walled mass. MRI has shown to be extremely useful in the diagnosis of complex pelvic masses. Currently, this is the most effective method for detecting and classifying fibroids considering the good resolution for demonstrating soft-tissues besides the capacity to depict the uterine anatomy(4). Zawin et al. have suggested that in uteri with > 140 cm3 complementary MRI studies would be convenient, considering that the presence of multiple nodules causing acoustic shadowing does not allow an adequate sonographic evaluation(6). Typically, leiomyomas present as circumscribed nodules, with hypointense signal in relation to the myometrium on T2-weighted sequences and contrast-enhancement on T1-weighted sequences. In cases where leiomyomas present an atypical appearance, MRI can better characterize the relationship between the mass and other pelvic structures besides providing a better definition of liquid and hemorrhagic components of the lesion(6). In the present case, the visualization of the uterine serosa covering the lesion has determined the origin of the mass, allowing the diagnosis and application of an appropriate therapy. Besides ovarian neoplasm(2,5), other differential diagnoses should be considered in the evaluation of complex pelvic masses in pregnant women, namely, endometriomas(7), abscesses(8), adenomyosis(4) and uterine leiomyosarcomas.
CONCLUSION The knowledge of differential diagnoses and respective US and MRI findings becomes indispensable, considering that fibroids with cystic degeneration may mimic a range of pelvic disorders. The finding of a thin myometrial layer covering the lesion establishes the definite diagnosis, allowing an appropriate therapeutic planning.
REFERENCES 1. Piazza MJ, Teixeira AC. Miomas e função reprodutora. Reprod Climat. 2002;17:91–3. [ ] 2. Fogata ML, Jain KA. Degenerating cystic uterine fibroid mimics an ovarian cyst in a pregnant patient. J Ultrasound Med. 2006;25:671–4. [ ] 3. Lev-Toaff AS, Coleman BG, Arger PH, et al. Leiomyomas in pregnancy: sonographic study. Radiology. 1987;164:375–80. [ ] 4. Murase E, Siegelman ES, Outwater EK, et al. Uterine leiomyomas: histopathologic features, MR imaging findings, differential diagnosis, and treatment. Radiographics. 1999;19:1179–97. [ ] 5. Sherer DM, Maitland CY, Levine NF, et al. Prenatal magnetic resonance imaging assisting in differentiating between large degenerating intramural leiomyoma and complex adnexal mass during pregnancy. J Matern Fetal Med. 2000;9: 186–9. [ ] 6. Zawin M, McCarthy S, Scoutt LM, et al. High-field MRI and US evaluation of the pelvis in women with leiomyomas. Magn Reson Imaging. 1990;8:371–6. [ ] 7. Reddy NM, Jain KA, Gerscovich EO. A degenerating cystic uterine fibroid mimicking an endometrioma on sonography. J Ultrasound Med. 2003;22:973–6. [ ] 8. Cohen JR, Luxman D, Sagi J, et al. Ultrasonic "honeycomb" appearance of uterine submucous fibroids undergoing cystic degeneration. J Clin Ultrasound. 1995;23:293–6. [ ] Received February 22, 2007. Accepted after revision April 9, 2007. * Study developed in the Unit of Echography at the Maternity Hospital of Hospital de Clínicas da Universidade Federal do Paraná (UFPR), Curitiba, PR, and Clínica DAPI – Diagnóstico Avançado por Imagem, Curitiba, PR, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554