Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 4 - July / Aug. of 2008
Vol. 41 nº 4 - July / Aug. of 2008
|
ORIGINAL ARTICLE
|
|
Air isodose curves in a mammography room |
|
|
Autho(rs): Maria Cecília Baptista Todeschini Adad, Gabriela Hoff, Elaine Evaní Streck, Rochele Lykawka |
|
|
Keywords: Radioprotection, Isodose curves, Mammography |
|
|
Abstract:
IMaster in Materials Engineering and Technology, Pontifícia Universidade Católica do Rio Grande do Sul (PUC-RS), Porto Alegre, RS, Brazil
INTRODUCTION Mammography is known as the most effective method for detecting non-palpable breast cancer(1,2), and has been routinely recommended for screening and extensively utilized both as regards to the number of patients as well as the number of times each patient is submitted do this procedure. The level of radiation exposure of both patient and technical team during mammographic examination is defined by the Portaria (Order) nº 453 issued by the Sanitary Vigilance Secretariat – Ministry of Health, Brazil, establishing that this exposure must be optimized, meaning that this exposure must be reduced to the lowest level possible(3). Additionally, as regards the patient absorbed dose during a radiological evaluation of the breast, this Portaria (Order) establishes that the skin entrance dose for a craniocaudal view should not exceed 10.0 mGy in a grid mammography and 4.0 mGy in a gridless mammography, considering a compressed breast with a thickness of 0.045 m for a screen-film system and a unit with anode and molybdenum filtration(3). These recommendations reflect the relevance of knowing the radiation scattering in the mammography room during the radiological examinationfor protection of the professionals, patients and general public. Among other studies already developed with similar purposes, the one developed by Vieira et al.(4) has determined isodose curves in brachytherapy for linear radioactive sources; Goulart et al.(5) and Andrade et al.(6) have estimated isodose curves in a hemodynamics room(5) for a digital fluoroscopy equipment besides the room where patients received iodine therapy(6) in nuclear medicine; and Fanti et al.(1) have developed a software for simulation of diagnostic radiography, allowing the construction of 3D images reflecting the entrance surface air kerma in a virtual patient. These data were compared with experimental information obtained by the same team with an anthropomorphic phantom and the aid of thermoluminescent dosimeters. In the present study, the distribution of absorbed dose in air in a mammography room was experimentally determined during the simulation of a mammographic examination, allowing the preparation of a 2D map demonstrating the doses distribution (isodose curves) at three different heights around the bucky, as well as the spatial localization of the sites in the room with higher absorbed dose in air. It is expected that these data can be useful in the planning of radiological protection for patients and professionals involved in the practice of mammography, as well as may shed light on the discussion about the calculation of shielding and utilization of individual protection equipment by the patients. Considering that the normal exposure rates for the general public must be restricted so that the effective yearly dose does not exceed 1 mSv(3), and that the limit for the equivalent level of environmental dose is 5 mSv/year in areas under control and 0.5 mSv/year in non-controlled areas, as far the planning for radiological protection barriers is concerned(3), also it is necessary to discuss the actual necessity of these barriers in mammography room, taking into consideration that the highest absorbed doses were recorded at sites corresponding to the organs of the patient.
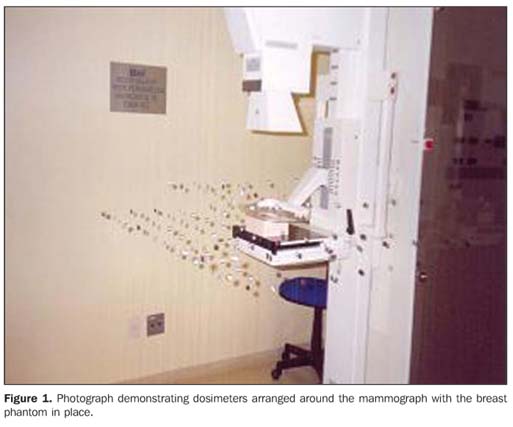
MATERIALS AND METHODS Data were collected at SIDI – Medicina por Imagem, Novo Hamburgo, RS, Brazil, in a room were a Senograph 600T Senix HF unit (GE Medical Systems; Buc Cedex, France) was installed. Mammographic examinations were simulated with a non-anthropomorphic, homogeneous distribution BR-12 breast phantom, representing a breast with 50% fat and 50% glandular tissue. Examinations were performed in compliance with the protocol and technique routinely utilized in the unit, i.e., Mo-Mo target-filter combination, AT 28 kVp and 77 mAs load. Measurements of absorbed dose in air were performed with 158 CaSO4 dosimeters duly identified, distributed over three rectangular grids with a 0.10 m horizontal spacing around the bucky, at three different heights: at the level of the bucky (z = 0.00 m), 0.10 m below the bucky (z = –0.10 m) and 0.10 m above the bucky (z = +0.10 m), as per Figure 1.
The dosimeters were attached with adhesive tape to wires hanging from the roof and their positioning coordinates (X, Y, Z) were noted down, so that the recorded dose was correctly associated with the respective positioning. Aiming at avoiding the interruption of the routine mammography unit operation and higher equipment wearing out, thermoluminescent dosimeters were selected for allowing the whole data collection in a single experiment, considering that tests performed with an ionization chamber had indicated the necessity of about 10 exposures for each point. Additionally, the option was for CaSO4 dosimeters appropriate to the voltage range utilized, without affecting the measurements reliability. After irradiation, the dosimeters were sent for reading by a specialized company, and the graphic representation of data regarding the distribution of absorbed dose in air around the bucky/phantom was prepared with the aid of an images processing software.
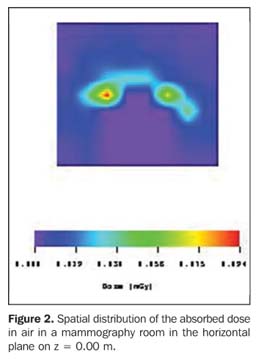
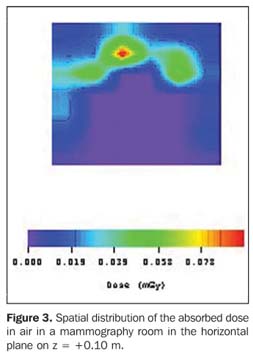
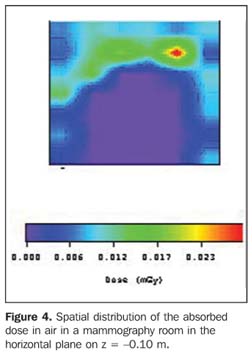
RESULTS The isodose curves representing the measurements of absorbed dose in air are shown on Figures 2, 3 and 4, respectively for heights of 0.10 m above the bucky and 0.10 m below the bucky.
The highest value for absorbed dose in air (8.3 ± 0.2) mGy was recorded on the center of the phantom surface (0.00; 0.10; 0.00) m focused by the primary beam. On the other hand, the lowest value for absorbed dose in air (0,008 ± 0.001) mGy was recorded on the most distant site reached by the primary beam (0.24; –0.30; 0.10) m. The Portaria (Order) 453 establishes that the skin entrance dose for a craniocaudal view should not exceed 10.0 mGy in a grid mammography and 4.0 mGy in a gridless mammography, considering a compressed breast with a thickness of 0.045 m for a screen-film system and a unit with anode and molybdenum filtration(3). Therefore, considering that the experiment described in the present study was performed with the grid, the highest value for absorbed dose in air is within the limits defined by the mentioned Portaria (Order) 453. Additionally, according to the American College of Radiology, the procedure recommended for determining the measurement of the breast entrance dose is positioning the ionization chamber on the X-ray field beside the breast phantom, at 0.040 m from the chest wall edge on the image receptor, and with the center of the chamber level with the top surface of the phantom(7). The highest values recorded for absorbed dose in air at the three different heights in relation to the bucky were (0.029 ± 0.001) mGy at (0.10; 0.27; –0.10) m, (0.097 ± 0.003) mGy at (0.14; –0.18; 0.10) m, and (0.094 ± 0.003) mGy at (0.00; –0.30; 0.0) m. An extra dosimeter was positioned on the lower surface of the bucky to evaluate its filtration degree. The measurements demonstrated a decrease of > 95% in the phantom entrance dose. Also, based on data demonstrated on Figures 2, 3 and 4, the authors could observe that, at the most distant sites, the values for accumulated absorbed dose after 10 exposures were bellow the dosimeters sensitivity threshold, so being recorded as zero.
DISCUSSION The data obtained show that, for a 0.41 m distance on the axis X (mammography bucky to the room door) and a 0.33 m distance on the axis Y (mammography bucky to the room walls), the estimated dose originating from the scattered radiation at the level z = 0.00 m corresponds to the background radiation. This evidence allows the discussion about the actual necessity of utilizing radiological protection barriers in a mammography room exceeding these dimensions. However, a definite decision should be based on additional tests with other view angles, projecting the primary beam directly towards the room door or walls. Also, it is necessary to take into consideration the financial cost for installing the mentioned barriers and that its project and construction would involve different professionals, including medical-physicists, architects and civil construction workers. The highest absorbed doses recorded for z = +0,10 m are shown on Figure 3 as red figures, and one of these regions is in front of the mammography unit, where the patients is positioned during the examination. For a woman who is approximately 1.70 tall (a median height), it is estimated that this would be the site of the thyroid gland. Considering that the thyroid is radiosensitive, periodic long exposures may contribute for the development of diseases like cancer. On its turn, as it can be seen on Figure 4, the region where the absorbed doses are higher at z = 0,10 m from the breast, is at the left side of the patient; and, based on these results, it is estimated that no radiosensitive organ would be affected. The analysis of these results emphasizes the relevance of radioprotection for the patient and, on the other hand, demonstrates that the situation in terms of room lay-out and occupational exposure is not critical, considering that the values for absorbed dose in air obtained for each angle of view are lower than 0.094 mGy for distance > 0.30 m, on the axis X for z = 0. However, it is important to note that these results were based only on the radiation scattered by the beam in a simulation of craniocaudal acquisition of mammographic images. Similar studies should be developed with the beam positioned for acquisition of oblique views, frequently utilized in mammography. It is important to note that, during horizontal or partially lateralized exposures, the bucky will act as a barrier against the primary beam radiation, resulting in scattering and significant reduction of the radiation that reaches the room walls.
CONCLUSIONS AND SUGGESTIONS The results of the present study indicate that the utilization of additional shielding in mammography rooms is not necessary, considering that at distances > 0.50m the measurements demonstrate an absorbed dose of < 0.1 mGy per exposure. Measurements performed under the bucky level have shown a significant decrease in the absorbed dose (> 95% as compared with the phantom entrance dose), so the shielding is effective in relation to the primary beam. Based on the irradiation geometry, no routine exposure is performed in the absence of the bucky. It is important to note that measurements were based on a single room lay-out, a single equipment and a single imaging view. These conclusions should be corroborated by further studies involving other routine imaging views and other mammography equipment, as well as different spectra and breast phantom thicknesses. Acknowledgements The authors thank Clínica SIDI – Medicina por Imagem for allowing data collection, and Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (Fapergs), for the financial support.
REFERENCES 1. Fanti V, Marzeddu R, Massazza G, et al. A simulator for X-ray images. Radiat Prot Dosimetry. 2005;114:350–4. [ ] 2. Goto S, Azuma Y, Sumimoto T, et al. Measurement of patient exposure dose on X-ray screening mammography. Instrumentation and Measurement Technology Conference, 2001. Proceedings of the 18th IEEE. 2001;1:191–6. [ ] 3. Brasil. Ministério da Saúde. Secretaria de Vigilância Sanitária. Diretrizes de proteção radiológica em radiodiagnóstico médico e odontológico. Portaria nº 453 de 1/6/1998. Diário Oficial da União. 1998 Jun 2;Seção 1. p. 7–16. [ ] 4. Vieira JW, Lima FRA, Kramer R. Determinação das curvas de isodose em braquiterapia com fontes radioativas lineares. Anais VI CBFM [CD-ROM]. Rio de Janeiro: VI Congresso Brasileiro de Física Médica; 2001. [ ] 5. Goulart AOS, Ferlin E., Bernasiuk MEB, et al. Determinação das curvas de isoexposição de um equipamento de fluoroscopia digital em uma sala de hemodinâmica. Anais VIII CBFM [CD-ROM]. Porto Alegre: VIII Congresso Brasileiro de Física Médica; 2003. [ ] 6. Andrade JRM, Ferlin EL, Spiro BL, et al. Determinação das curvas de isoexposição em pacientes submetidos à iodoterapia. Anais VIII CBFM [CD-ROM]. Porto Alegre: VIII Congresso Brasileiro de Física Médica; 2003. [ ] 7. Ng KH, Aus RJ, DeWerd LA, et al. Entrance skin exposure and mean glandular dose: effect of scatter and field gradient at mammography. Radiology. 1997;205:395–8. [ ] Received February 5, 2007. Accepted after revision November 12, 2007. * Study developed at Faculdade de Física da Pontifícia Universidade Católica do Rio Grande do Sul (PUC-RS), Porto Alegre, RS, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554