Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 5 - Sep. / Oct. of 2009
Vol. 42 nº 5 - Sep. / Oct. of 2009
|
CASE REPORT
|
|
Metastatic melanoma causing small bowel intussusception: diagnosis by 18F-FDG PET/CT |
|
|
Autho(rs): Frederico Ferreira de Souza, Felipe Ferreira de Souza, Daniel Andrade Tinoco de Souza, Ciaran Johnston |
|
|
Keywords: PET/CT, Melanoma, Intussusception |
|
|
Abstract:
IFellow in Oncoradiology, Dana Farber Cancer Institute/Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA
INTRODUCTION Malignant melanoma is a common tumor whose incidence is increasing, representing 1–3% of all cancers in the United States(1). Gastrointestinal metastases caused by melanoma may present as mucosal, submucosal lesions, or as serous implants(2). Metastases are more frequently found in the mesentery and distal small bowel than in the proximal gastrointestinal tract or in the colon. Previous studies have evidenced that combined positron emission tomography (PET) and computed tomography (CT) – PET/CT is a reliable method that has shown to be superior to pure PET or CT in the detection and differentiation of visceral metastases from melanoma(3,4). The present study is aimed at demonstrating 18F-FDG PET/CT findings of a metastatic lesion in the small bowel originated from melanoma, and highlighting the importance of this method in the detection of metastatic sites, which may not be seen when only CT is used for staging or restaging purpose.
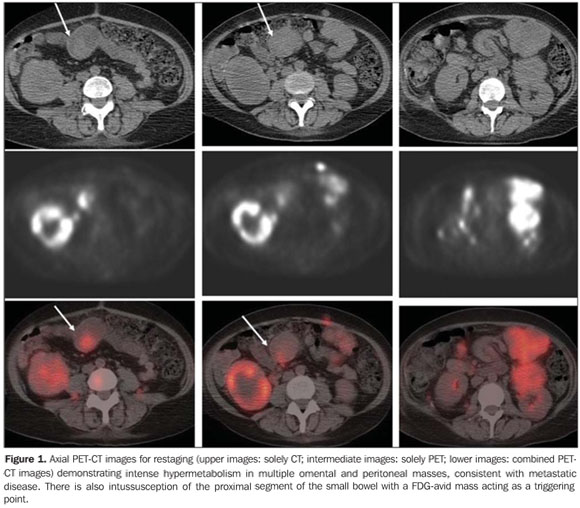
CASE REPORT A 48-year-old female patient with history of stage IV metastatic ocular melanoma, submitted to a PET/CT study for restaging of the disease. Approximately 60 minutes after intravenous injection of radiopharmaceutical (18F-FDG), a PET scan was performed from the skull base to the proximal portion of the thighs. Additional PET images of the lower limbs were also obtained in accordance with the department's protocol. The patient was normoglycemic at the moment of the 18F-FDG injection. The PET study demonstrated focal lesions with increased radiopharmaceutical uptake in the neck, chest, abdomen and pelvis, as well as in the lower and upper extremities, and in the subcutaneous tissue, corresponding to multiple metastatic sites. Additionally, the FDG-PET images demonstrated a focal area of radiopharmaceutical uptake in the mesogastric region, which, after correlation with CT, was shown to be located in the small bowel (Figure 1). CT images also demonstrated proximal bowel invagination into the distal intestinal bowel, and an area of intraluminal eccentric adipose density, contiguous with the mesenteric fat. An enhancing metastatic lesion (maximum SUV: 6.0) acted as the initial point of the intussusception. There were no definite signs of intestinal obstruction in this study and on a control CT performed 30 days afterwards. The patient received palliative treatment and died after three months.
DISCUSSION Metastatic melanoma in the gastrointestinal tract is relatively uncommon. However, it represents approximately one third of the metastases to the gastrointestinal tract, being found in 58% of the autopsies of patients with melanoma(4). The ante-mortem diagnosis is achieved in only 1.5–4.4% of all patients with melanoma, and the lesions are more commonly found in the jejunum and distal ileum than in the proximal small bowel. The location of hematogenous deposition of neoplastic cells influences the radiological aspect of the metastasis. Deposition in the submucosal layer, for example, results in intraluminal mass; deposits in the serous layer result in implants which, as the mass grows, may progressively compress the adjacent bowel; deposition in the mesentery results in masses that, when extremely large, cause significant compression of the small bowel(5). Traditionally, the possibility of metastatic melanoma in the small bowel has been in general considered when a "target lesion" is demonstrated by imaging studies of the small bowel(3). However, recent studies indicate that melanoma shall be included in the differential diagnosis whenever cavitary, infiltrating or polypoid lesions are found in the small bowel(4). Intussusception of the small bowel secondary to metastatic lesion from melanoma has already been described in the literature, and its presentation is variable(6). The typical sign of intussusceptions is a segment of the intestinal loop "telescoping" inside another. Common clinical symptoms that may be present in patients with a history of metastatic melanoma in the intestinal tract include abdominal pain and/or anemia. When such symptoms are present a thorough clinical and radiological investigation of chronic abdominal pain complaints and anemia(7) is necessary. Patients with visceral melanoma metastases are generally treated with systemic chemotherapy, with a mean survival of only 5 to 11 months, depending on the metastasis site(7). Traditionally, surgical intervention for metastatic lesions to the gastrointestinal tract is reserved for symptomatic lesions causing obstruction or bleeding. However, a study with a larger sample of patients with melanoma and ante-mortem diagnosis of metastasis to the gastrointestinal tract(7) has shown that in the subgroup of patients with stage IV disease, the mean survival can be extended by means of curative abdominal surgery. For this reason, the radiological investigation plays an significant role in determining the origin of the problem. Bender et al. have evaluated patterns of metastases to the small bowel in 32 patients with pathologically confirmed metastatic melanoma. The authors have demonstrated that the most commonly used imaging methods, such as intestinal transit and conventional CT, are not reliable for demonstrating melanoma metastasis to the small bowel(4,8). PET, in spite of providing high sensitivity and specificity in the detection of visceral metastasis from melanoma, presents low accuracy in the detection of lymph node metastasis and pulmonary metastatic lesions smaller than 10 mm(3). However, for determining the extent of primary non-small cell lung cancer, FDG PET/CT has shown to be a better method than CT, being considered by some as "indispensable" in the radiotherapy planning(9). The use of FDG PET/CT has a large clinical impact on patients with melanoma. This method has been utilized in some institutions as the method of choice for detecting and differentiating metastases in areas otherwise inaccessible by physical examination and biopsy. Patients with metastatic melanoma to the gastrointestinal tract may benefit from curative resection and, therefore, it is of great importance that the diagnosis be made at an early stage of the disease(10). The 18F-FDG PET/CT is a highly reliable method for the detection of melanoma metastases and it appears to be superior to other conventional imaging methods and PET(3). The present case demonstrated a significant contribution of dual modality 18FDG PET/CT for detection and localization of intestinal metastatic lesion, which could have gone undetected at CT, or erroneously related to abdominal structures adjacent to the small bowel, in the case of isolated utilization of PET. The images fusion allowed by PET/CT provided for a correct and topographically accurate diagnosis of the intestinal intussusception in a patient with diffuse metastatic melanoma submitted to PET/CT scan for restaging purposes.
REFERENCES 1. Adam YG, Efron G. Cutaneous malignant melanoma: current views on pathogenesis, diagnosis, and surgical management. Surgery. 1983;93:481–94. [ ] 2. Kawashima A, Fishman EK, Kuhlman JE, et al. CT of malignant melanoma: patterns of small bowel and mesenteric involvement. J Comput Assist Tomogr. 1991;15:570–4. [ ] 3. Reinhardt MJ, Joe AY, Jaeger U, et al. Diagnostic performance of whole body dual modality 18F-FDG PET/CT imaging for N- and M-staging of malignant melanoma: experience with 250 consecutive patients. J Clin Oncol. 2006;24:1178–87. [ ] 4. Bender GN, Maglinte DD, McLarney JH, et al. Malignant melanoma: patterns of metastasis to the small bowel, reliability of imaging studies, and clinical relevance. Am J Gastroenterol. 2001;96:2392–400. [ ] 5. McDermott VG, Low VH, Keogan MT, et al. Malignant melanoma metastatic to the gastrointestinal tract. AJR Am J Roentgenol. 1996;166:809–13. [ ] 6. Strobel K. Small intestine invagination in metastatic intestinal malignant melanoma. Rofo. 2001;173:768–9. [ ] 7. Ollila DW, Essner R, Wanek LA, et al. Surgical resection for melanoma metastatic to the gastrointestinal tract. Arch Surg. 1996;131:975–80. [ ] 8. Prabhakar HB, Sahani DV, Fischman AJ, et al. Bowel hot spots at PET-CT. Radiographics. 2007;27:145–59. [ ] 9. Faria SL, Lisbona R, Stern J, et al. O uso de FDG-PET/TC scan no planejamento da radioterapia em câncer do pulmão não de pequenas células. Radiol Bras. 2007;40:345–8. [ ] 10. Tatlidil R, Mandelkern M. FDG-PET in the detection of gastrointestinal metastases in melanoma. Melanoma Res. 2001;11:297–301. [ ]
Received February 28, 2008. Accepted after revision May 9, 2008.
* Study developed at Dana Farber Cancer Institute, Harvard Medical School, Boston, MA, USA. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554