Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Ahead of Print
Ahead of Print
|
NEWS IN RADIOLOGY
|
|
Percutaneous cholangioscopy for the treatment of choledocholithiasis |
|
|
Autho(rs): Tiago Kojun Tibana1; Renata Motta Grubert2; Carlos Marcelo Dotti Rodrigues da Silva3; Vinícius Adami Vayego Fornazari4; Thiago Franchi Nunes5 |
|
|
INTRODUCTION
Most cases of choledocholithiasis require some type of surgical treatment. Laparoscopy, endoscopic retrograde cholangiopancreatography, transhepatic cholangiography, and open surgery are the most widely used treatment methods(1). The choice will depend on the clinical status of the patient, as well as on morphological characteristics and location of the stones. Approximately 90% of gallstones are treated with endoscopic retrograde cholangiopancreatography(2). However, when that technique fails—because of factors such as the stones being large or in an atypical location; anatomical abnormalities of the hepatopancreatic ampulla; duodenal diverticulum; sequelae of liver transplantation; and a history of gastric surgery requiring Roux-en-Y gastric shunting—other modalities should be used(3). As endoscopic materials improved, percutaneous lithotripsy and ureteroscopy appeared as good options for the treatment of renal and ureteral calculi, respectively. In line with this evolution and the improvements in the technical skills of surgeons and interventional radiologists, a multidisciplinary approach to patient care allowed these modalities to be more widely used and applied in different situations, such as in cases of choledocholithiasis(1). Recent technological developments have led to the appearance of small-caliber, flexible devices and new energy sources for the fragmentation of stones, which, combined with expertise in urological endoscopy and interventional radiology, represent promising options for solving complex gallstone cases or for replacing conventional techniques when these fail or cannot be performed(4–8). Although urological endoscopy techniques can be used for the treatment of bile duct stones, their indications have yet to be well established(9,10). Here, we describe an interventional radiology procedure performed with a flexible ureteroscope and a Holmium:YAG laser for the removal of complex gallstones (Figure 1). 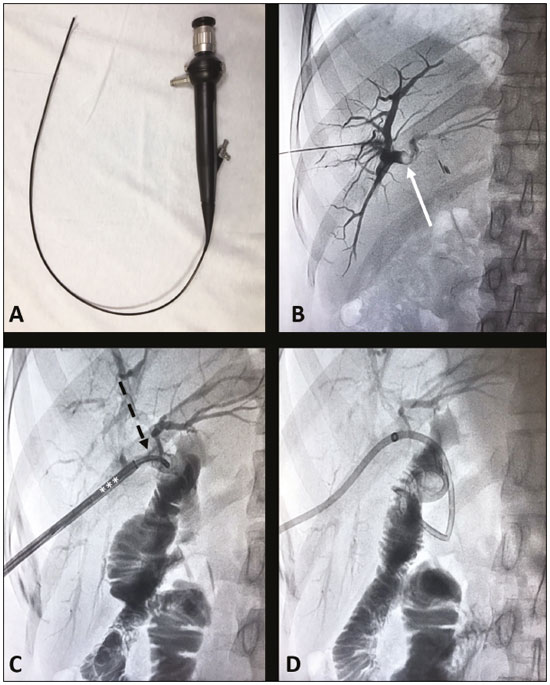 Figure 1. A: Flexible fiberoptic endoscope. B: Cholangiography showing obstruction of the biliary tract by an intrahepatic gallstone (arrow). C: Fiberoptic endoscope (dashed arrow) positioned inside the 10F sheath (asterisks), adjacent to the stone. D: Fluoroscopy showing no signs of remnant gallstone fragments and confirming the correct positioning of the external drainage tube. PROCEDURE The procedure starts with fluoroscopy-guided puncture of the (right or left) bile duct based on previous imaging tests. Cholangiography with right anterior oblique projection is then performed for better planning of the procedure. Direct visualization of the stone is provided by a 7.5F flexible fiberoptic endoscope, introduced through a 10F × 35 cm sheath. A 0.9% sodium chloride solution at a pressure of 200 mmHg is used for continuous irrigation. The fragmentation of the gallstones is performed with a 200 µm fiber laser, at 0.6–1.0 J/pulse and a frequency of 6–10 Hz. Stone fragments are cast into the duodenum or removed with a nitinol basket. At the end of the procedure, a control cholangiography is performed to confirm there are no intrahepatic gallstone fragments remaining. At our center, an external biliary drainage tube is put in place and patients are discharged within 48 h. After 60 days, the drainage tube is replaced with a larger one (the 10F tube is replaced with a 12F tube and, later, with a 14F tube). After 6–9 months, if there are no stones remaining, the tubes are finally removed. REFERENCES 1. Ponsky LE, Geisinger MA, Ponsky JL, et al. Contemporary “urologic” intervention in the pancreaticobiliary tree. Urology. 2001;57:21–5. 2. Williams E, Beckingham I, El Sayed G, et al. Updated guideline on the management of common bile duct stones (CBDS). Gut. 2017;66:765–82. 3. Rimon U, Kleinmann N, Bensaid P, et al. Percutaneous transhepatic endoscopic holmium laser lithotripsy for intrahepatic and choledochal biliary stones. Cardiovasc Intervent Radiol. 2011; 34:1262–6. 4. Gamal EM, Szabó A, Szüle E, et al. Percutaneous video choledochoscopic treatment of retained biliary stones via dilated T-tube tract. Surg Endosc. 2001;15:473–6. 5. Hazey JW, McCreary M, Guy G, et al. Efficacy of percutaneous treatment of biliary tract calculi using the holmium:YAG laser. Surg Endosc. 2007;21:1180–3. 6. Shamamian P, Grasso M. Management of complex biliary tract calculi with a holmium laser. J Gastrointest Surg. 2004;8:191–9. 7. Zurstrassen CE, Bitencourt AGV, Guimaraes MD, et al. Percutaneous stent placement for the treatment of malignant biliary obstruction: nitinol versus elgiloy stents. Radiol Bras. 2017;50:97–102. 8. Cardarelli-Leite L, Fornazari VAV, Peres RR, et al. The value of percutaneous transhepatic treatment of biliary strictures following pediatric liver transplantation. Radiol Bras. 2017;50:308–13. 9. Adamek HE, Maier M, Jakobs R, et al. Management of retained bile duct stones: a prospective open trial comparing extracorporeal and intracorporeal lithotripsy. Gastrointest Endosc. 1996;44:40–7. 10. Wolf JS Jr, Nakada SY, Aliperti G, et al. Washington University experience with extracorporeal shock-wave lithotripsy of pancreatic duct calculi. Urology. 1995;46:638–42. 1. Hospital Universitário Maria Aparecida Pedrossian da Universidade Federal de Mato Grosso do Sul (HUMAP-UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0001-5930-1383 2. Hospital Universitário Maria Aparecida Pedrossian da Universidade Federal de Mato Grosso do Sul (HUMAP-UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0001-6713-2575 3. Santa Casa de Campo Grande, Campo Grande, MS, Brazil; https://orcid.org/0000-0002-4483-0685 4. Escola Paulista de Medicina da Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil; https://orcid.org/0000-0002-5880-1703 5. Hospital Universitário Maria Aparecida Pedrossian da Universidade Federal de Mato Grosso do Sul (HUMAP-UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0003-0006-3725 Correspondence: Dr. Thiago Franchi Nunes Avenida Senador Filinto Müller, 355, Vila Ipiranga Campo Grande, MS, Brazil, 79080-190 Email: thiagofranchinunes@gmail.com Received 11 May 2018 Accepted after revision 6 July 2018 Publication date: 05/08/2019 |
|
GN1© Copyright 2024 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554