Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Ahead of Print
Ahead of Print
|
NEWS IN RADIOLOGY
|
|
Pulmonary nodule localization guided by computed tomography using a nitinol guidewire before video-assisted thoracoscopic surgery |
|
|
Autho(rs): Tiago Kojun Tibana1; Tony Rocha de Carvalho2; Adalberto Arão Filho3; Edson Marchiori4; Thiago Franchi Nunes5 |
|
|
INTRODUCTION
Image-guided puncture techniques are being used with increasing frequency in interventional radiology(1–4). The appropriate management of a pulmonary nodule usually requires a definitive pathological diagnosis. The accuracy of computed tomography (CT)-guided biopsy is significantly lower for small pulmonary nodules than for nodules > 1 cm(5). Although minimally invasive video-assisted thoracoscopic surgery has come to be widely used for the diagnosis of small lesions, it is difficult for the surgeon to determine the exact location during surgery if the nodules are small and are located more than 2 cm from the pleural surface(6). If they are deeper in the lung, palpation is necessary in order to locate them for excision(7). For all other nodules that are potentially resectable through video-assisted thoracoscopic surgery, the preoperative location should be considered(8). There have been reports of various nodule localization techniques employing markers such as spiral hookwires, contrast media, cyanoacrylate, and methylene blue(9). Localization using hookwires has been reported in larger studies, sometimes being performed in combination with methylene blue injection and sometimes being used in children(10–12). Most of these marker systems have been customized for use in lung tissue or were not specifically designed for such use, having rather been designed for the localization of breast lesions. Because of the difficulty in locating a pulmonary nodule intraoperatively and the increasing role that CT plays in identifying such nodules in clinical lung cancer screening, there has been extensive investigation to improve localization techniques in order to facilitate the resection of small nodules during video-assisted thoracoscopic surgery(8). The marker system consists of an 18 G coaxial needle, an insertion device, and a nitinol hookwire. The hookwire can be repositioned if necessary, and the spiral tip provides firm anchoring in the lung tissue (Figure 1). 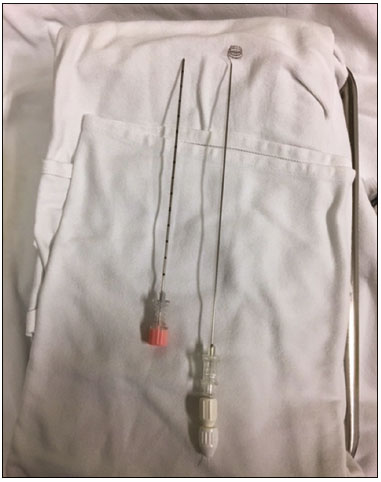 Figure 1. Nodule marker system composed of a coaxial needle and hookwire. PROCEDURE Depending on the location of the nodule (Figure 2), patients are positioned in the CT scanner in such a way as to achieve a better assessment of the depth of the lesion, as well as to optimize the hookwire placement and angulation—in the supine, prone, or oblique position. 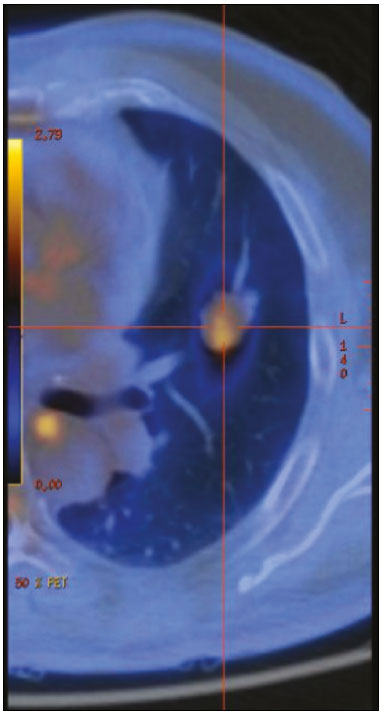 Figure 2. Axial PET/CT showing a pulmonary nodule with soft-tissue density and lobulated contours, located in the upper lobe of the left lung, with a SUVmax of 2.19. After local infiltration with 2% lidocaine, the coaxial needle is inserted, under CT guidance, adjacent to or within the nodule, on the basis of an analysis made by a multidisciplinary team (comprising an interventional radiologist, a nuclear physician, and a thoracic surgeon). Upon withdrawal of the mandrel, the insertion device is used in order to implant the hookwire marker. The deployment requires no rotational movement. Before removing the coaxial needle and the insertion device, the correct position of the marker and the angle between the introducing needle and the pleural surface should be confirmed (Figure 3). Subsequently, a second CT scan is acquired to identify any immediate complications, such as pneumothorax and hematoma, or any other additional finding. Finally, the distance from the spiral tip to the intended target is evaluated. 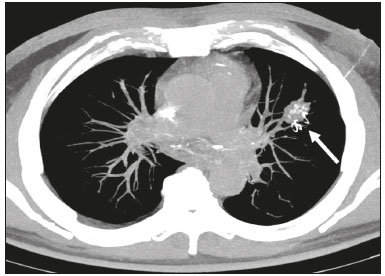 Figure 3. Axial MIP CT reconstruction showing the hookwire positioning, adjacent to the nodule with coarse calcifications (arrow). After implantation of the hookwire, the patient is transported directly to the preoperative holding area. Any complaints are documented, and a brief report of the procedure, together with copies of the relevant CT images, is sent to the operating room. After video-assisted thoracoscopic surgery and excision of the nodule (Figure 4), the surgeon fills out a form documenting the position and accuracy of the guidewire location and a brief assessment of the system used.  Figure 4. Macroscopic aspect of the surgical specimen (nodule) and hookwire marker. REFERENCES 1. Zurstrassen CE, Bitencourt AGV, Guimaraes MD, et al. Percutaneous stent placement for the treatment of malignant biliary obstruction: nitinol versus elgiloy stents. Radiol Bras. 2017;50:97–102. 2. Schiavon LHO, Tyng CJ, Travesso DJ, et al. Computed tomography-guided percutaneous biopsy of abdominal lesions: indications, techniques, results, and complications. Radiol Bras. 2018;51:141–6. 3. Carneiro GAC, Arantes Pereira FP, Lopes FPPL, et al. Magnetic resonance imaging-guided vacuum-assisted breast biopsy: experience and preliminary results of 205 procedures. Radiol Bras. 2018;51:351–7. 4. Bitencourt AGV, Graziano L, Guatelli CS, et al. Ultrasound-guided biopsy of breast calcifications using a new image processing technique: initial experience. Radiol Bras. 2018;51:106–8. 5. Shaffer K. Role of radiology for imaging and biopsy of solitary pulmonary nodules. Chest. 1999;116(6 Suppl):519S–522S. 6. Hsu HH, Shen CH, Tsai WC, et al. Localization of nonpalpable pulmonary nodules using CT-guided needle puncture. World J Surg Oncol. 2015;13:248. 7. Hochhegger B, Perin FA, Camargo SM, et al. Ground-glass nodules and CT-guided placement of platinum coils. J Bras Pneumol. 2014;40:450–2. 8. Tyng CJ, Baranauskas MVB, Bitencourt AGV, et al. Preoperative computed tomography-guided localization of ground-glass opacities with metallic clip. Ann Thorac Surg. 2013;96:1087–9. 9. Partik BL, Leung AN, Müller MR, et al. Using a dedicated lung-marker system for localization of pulmonary nodules before thoracoscopic surgery. AJR Am J Roentgenol. 2003;180:805–9. 10. Tyng CJ, Schiavon LHO, Coimbra FJF, et al. Modified preoperative computed tomographic-guided localization of colorectal liver metastases with metallic clips—technical note. Clin Colorectal Cancer. 2015;14:123–7. 11. Kleedehn M, Kim DH, Lee FT, et al. Preoperative pulmonary nodule localization: a comparison of methylene blue and hookwire techniques. AJR Am J Roentgenol. 2016;207:1334–9. 12. Parida L, Fernandez-Pineda I, Uffman J, et al. Thoracoscopic resection of computed tomography-localized lung nodules in children. J Pediatr Surg. 2013;48:750–6. 1. Hospital Universitário Maria Aparecida Pedrossian da Universidade Federal de Mato Grosso do Sul (HUMAP-UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0001-5930-1383 2. Hospital Universitário Maria Aparecida Pedrossian da Universidade Federal de Mato Grosso do Sul (HUMAP-UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0003-4865-2924 3. MS Diagnósticos Médicos, Campo Grande, MS, Brazil; https://orcid.org/0000-0002-4799-2700 4. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil; https://orcid.org/0000-0001-8797-7380 5. Hospital Universitário Maria Aparecida Pedrossian da Universidade Federal de Mato Grosso do Sul (HUMAP-UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0003-0006-3725 Correspondence: Dr. Thiago Franchi Nunes Avenida Senador Filinto Müller, 355, Vila Ipiranga Campo Grande, MS, Brazil, 79080-190 Email: thiagofranchinunes@gmail.com Received 15 March 2018. Accepted after revision 2 May 2018. |
|
GN1© Copyright 2024 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554